Small sharp spikes; wading into the controversy.
Aug 03, 2025When Gibbs and Gibbs first drew attention to these waves in 1952, because they were commonly seen in patients with epilepsies, they classified these discharges as epileptiform in nature. However, their observations were subject to considerable selection biases. For the past five decades or so these discharges have generally been considered benign and most standard texts state as much. There have been numerous studies that support this hypothesis. This is but one, from Timothy Pedley and his co-authors. Benign epileptiform transients of sleep. Clarification of the small sharp spike controversy - PubMed. In 120 healthy volunteers, with no risk factors for the development of seizures and without any history suggestive of epileptic seizures, small sharp spikes were present in 24% of patients subjected to 24-hour sleep deprived EEG recordings, similar to the prevalence of 20% of 599 unselected hospital patients. This suggests that these Small sharp spikes lack specificity for the diagnosis of epilepsy. However, others have pointed out that these recordings included nasopharyngeal electrodes and that the definition of small sharp spikes was slightly different to the generally accepted definition. Remarkably, there is only one other study that has systematically evaluated benign discharges on the scalp EEG recordings of healthy individuals; this study was limited to young, healthy pilots and standard EEG recordings only. Prevalence of benign epileptiform variants during initial EEG examination in French military aircrew - PubMed
As shown in previous posts, there are ways of distinguishing low amplitude spikes (in other words, inter-ictal epileptiform discharges) from small sharp spikes. Small sharp spikes re defined by the following criteria:
1. monophasic or biphasic electronegative spikes
2. a duration less than 50 milliseconds and
3. amplitude less than 50 mV
4. a subtle postspike slow wave may be present.
5. they are predominantly observed during drowsiness and light sleep
6. they have a large field, primarily located unilaterally or bilaterally in the temporal regions.
Here are a few articles, including one from Barbara Westmoreland and Donald Klass, discussing benign variants. If nothing else, click on these and read the abstracts. Some of these have links to the full articles.
EEG normal variants: A prospective study using the SCORE system - PubMed
The above used a computer-based algorithm for classifying discharges, improving the consistency of classification. Most studies, including the following more recent articles, rely on "expert" electroencephalographers to classify discharges. Here is a relatively recent publication in the reputable Journal of Clinical Neurophysiology
Normal Variants Are Commonly Overread as Interictal Epileptiform Abnormalities - PubMed
And here are several other articles on the subject:
Nonepileptogenic epileptiform electroencephalographic activity - PubMed
Benign epileptiform variants in EEG: A comprehensive study of 3000 patients - PubMed
Prevalence of benign epileptiform variants from an EEG laboratory in India and frequency of their misinterpretation - PubMed
Prevalence of benign epileptiform variants - PubMed
There have been challenges to the above dominant hypothesis about small sharp spikes, with some studies suggesting an association between small sharp spikes and epilepsy. There are some older studies:
Small sharp spikes revisited: further data on this controversial pattern - PubMed
Small sharp spikes: possible relationship to epilepsy - PubMed
and here is a more recent one:
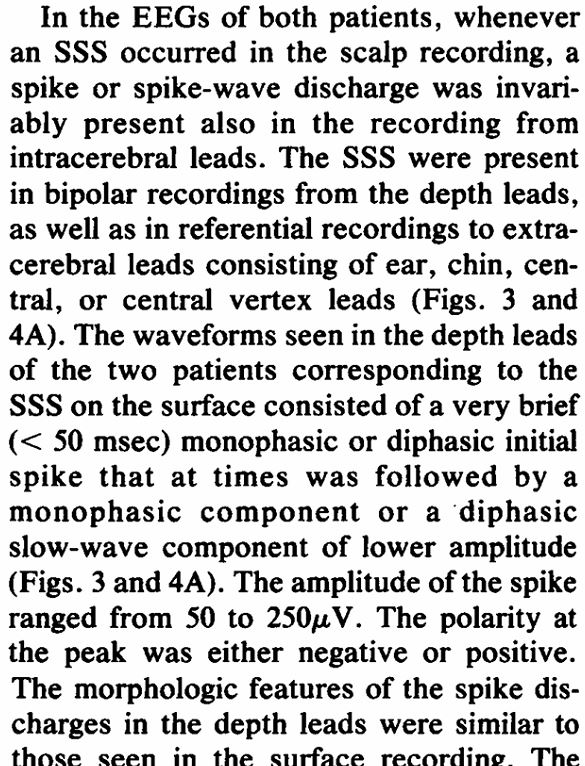
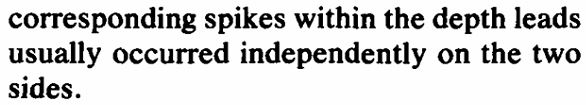
The above study has a historical context. In 1970, Barbara Westmoreland, Jean Reiher and Donald Klass described 2 patients whose small sharp spikes on scalp EEG recordings were time-locked to spikes in the medial temporal lobes of patients with medial temporal lobes epilepsy studied with depth electrodes. You may appreciate how these astute observations by leading electroencephalographers provided the basis for further study decades later. Westmoreland and her co-authors observed the following:
They found no evidence that small sharp spikes were related to the process of epileptogenesis, since these small sharp spikes occurred in areas independent of those generating spontaneous seizures and after-discharges, and stimulation did not alter these small sharp spikes, either in their frequency or their morphology.
In their discussion they conclude:
The authors of The clinical significance of small sharp spikes: A retrospective study of 909 patients in epilepsy monitoring unit - PubMed took the findings of the above study one step further by looking at the temporal association between these discharges on scalp EEG with spikes in the medial temporal lobe on intracranial EEG recordings, which they reported here Small sharp spikes as EEG markers of mesiotemporal lobe epilepsy - PubMed
The above studies formed the basis for a review by Issa et al. in the Journal of Clinical Neurophysiology, which you can find here Clinical Implications of Small Sharp Spikes in Mesial Temporal Lobe Epilepsy: Controversies and Opportunities - PubMed
There was an excellent letter from Richard Wennberg in response to this article:
Which small sharp spikes are benign epileptiform transients of sleep? - PubMed
Wennberg draws attention to EEG features, albeit quite technical, that they have found to distinguish small sharp spikes from inter-ictal epileptiform discharges.
Here is the reply to the above letter:
Reply to "which small sharp spikes are benign epileptiform transients of sleep?" - PubMed
In this article Clinical Implications of Small Sharp Spikes in Mesial Temporal Lobe Epilepsy: Controversies and Opportunities - PubMed, Issa et al. raise the possibility that small sharp spikes might be a biomarker for "latent medial temporal lobe epilepsy". If this hypothesis is correct, and it is still a big if, it may foster studies that attempt to interrupt the process of epileptogenesis in the medial temporal lobe. Irrespective of these articles, you should still continue to report these as benign discharges, especially as these discharges clearly may occur in people without epilepsy. To reiterate, specificity is not something that you want to forego when reporting an EEG.
You will notice that the articles about this subject come from the same set of authors, but at least their hypothesis is based on scientific study and their observations have precedent in the form of the 2 case reports from 1970. I find it difficult to conceptualise how these low amplitude discharges with such a large field in the brain might be biomarkers of a process of epileptogenesis in the medial temporal lobe, which is remote from scalp EEG electrodes. There will no doubt be more studies on the subject, so watch this space.