ICU, "Not waking up, seizures? Brain dead?"
Aug 26, 2025This is a common problem. What would you tell the clinician in your clinical interpretation about the EEG?
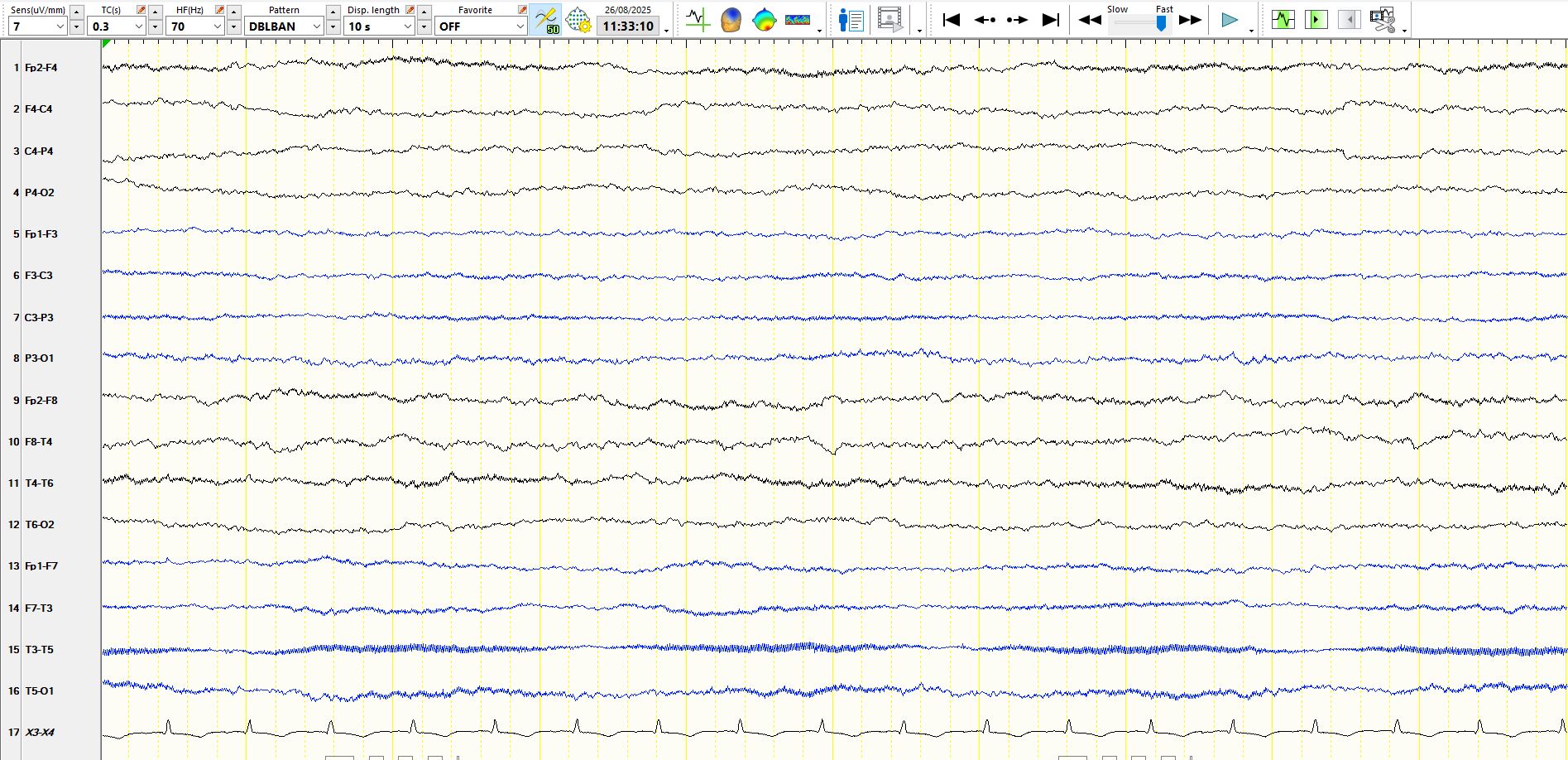
Figure 1. Bipolar anterior-posterior montage, 7 µV per millimetre:
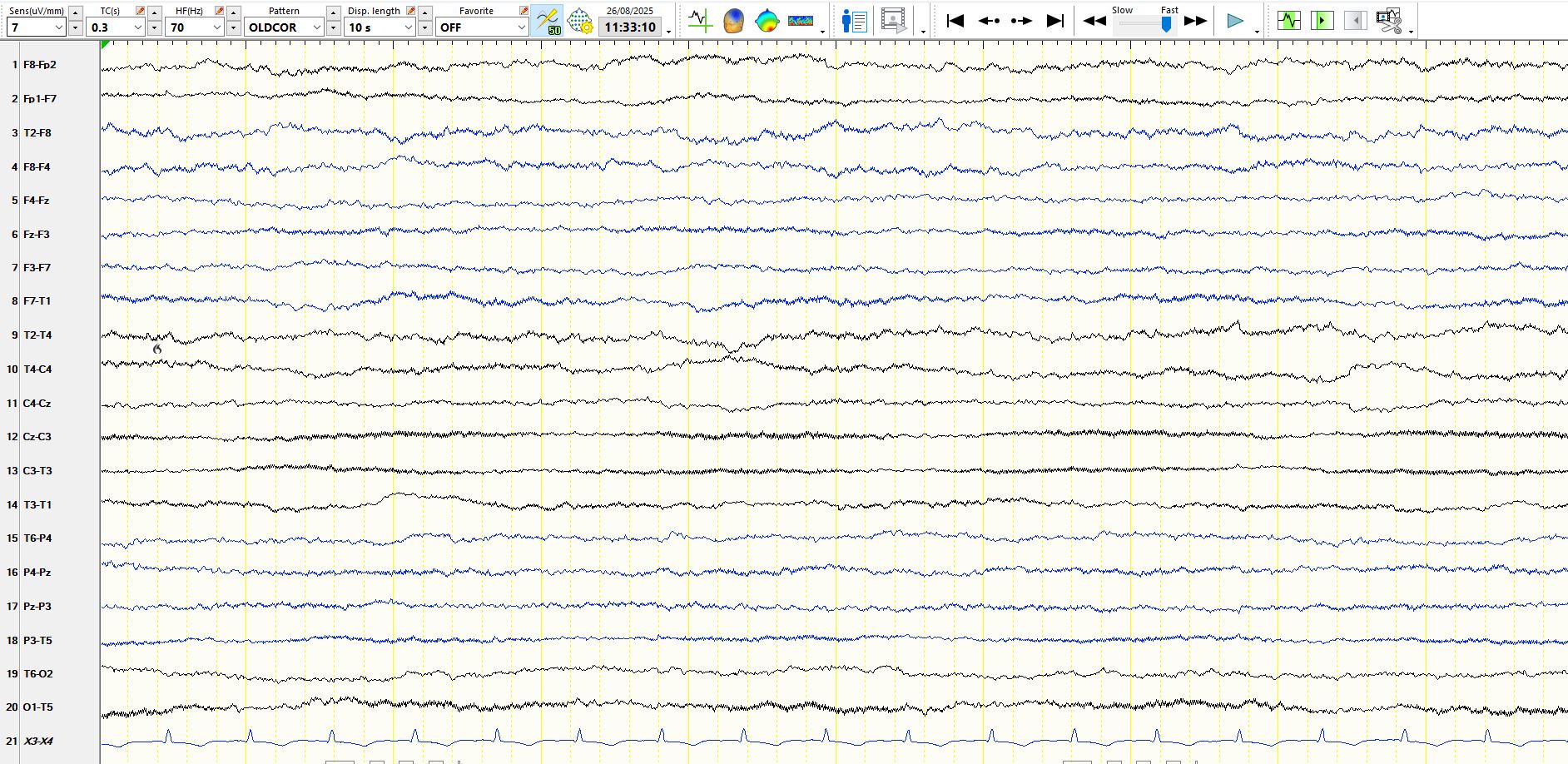
Figure 2. Coronal montage, 7 µV per millimetre:
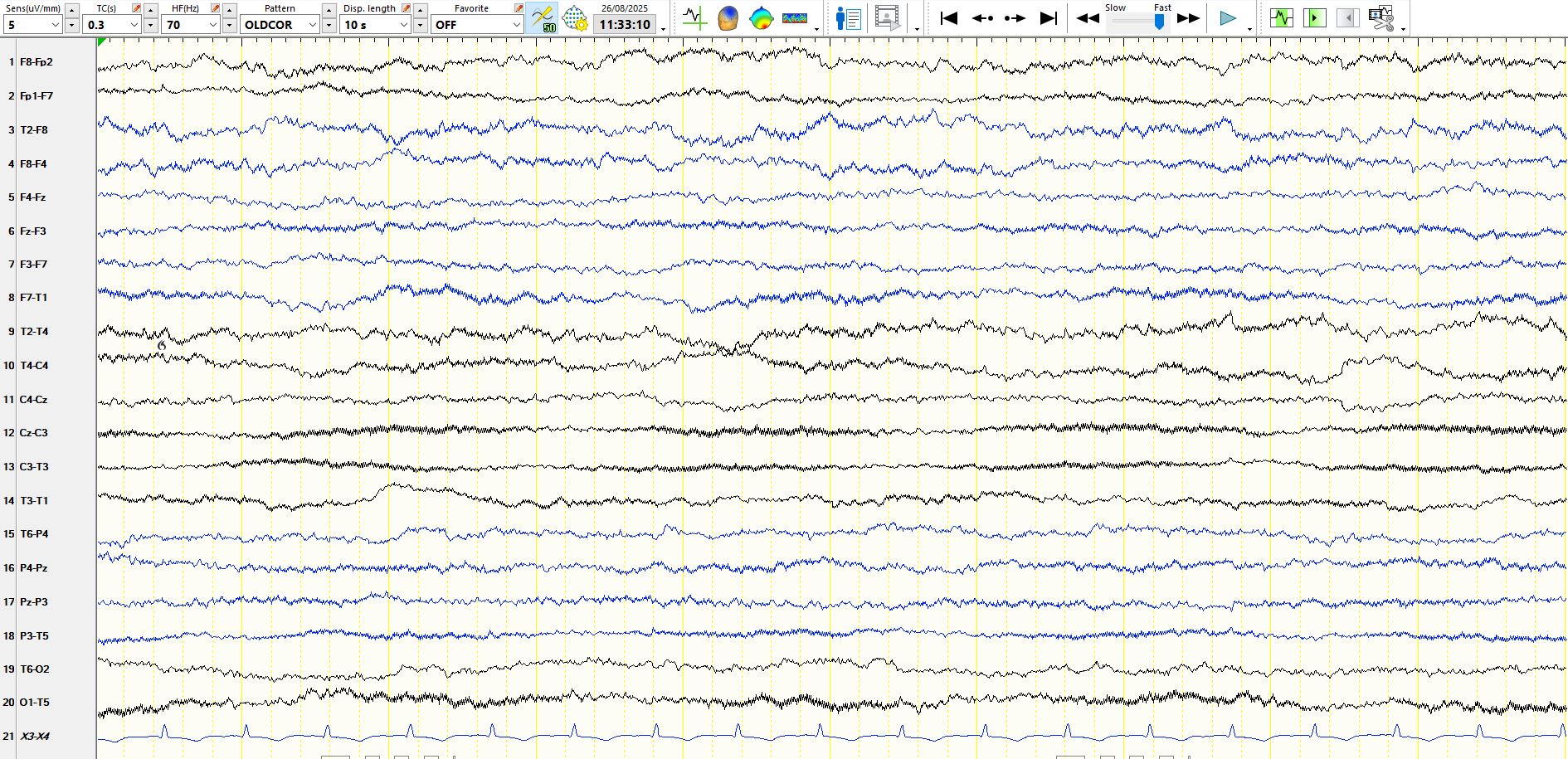
Figure 3. Coronal montage, 5 µV per millimetre:
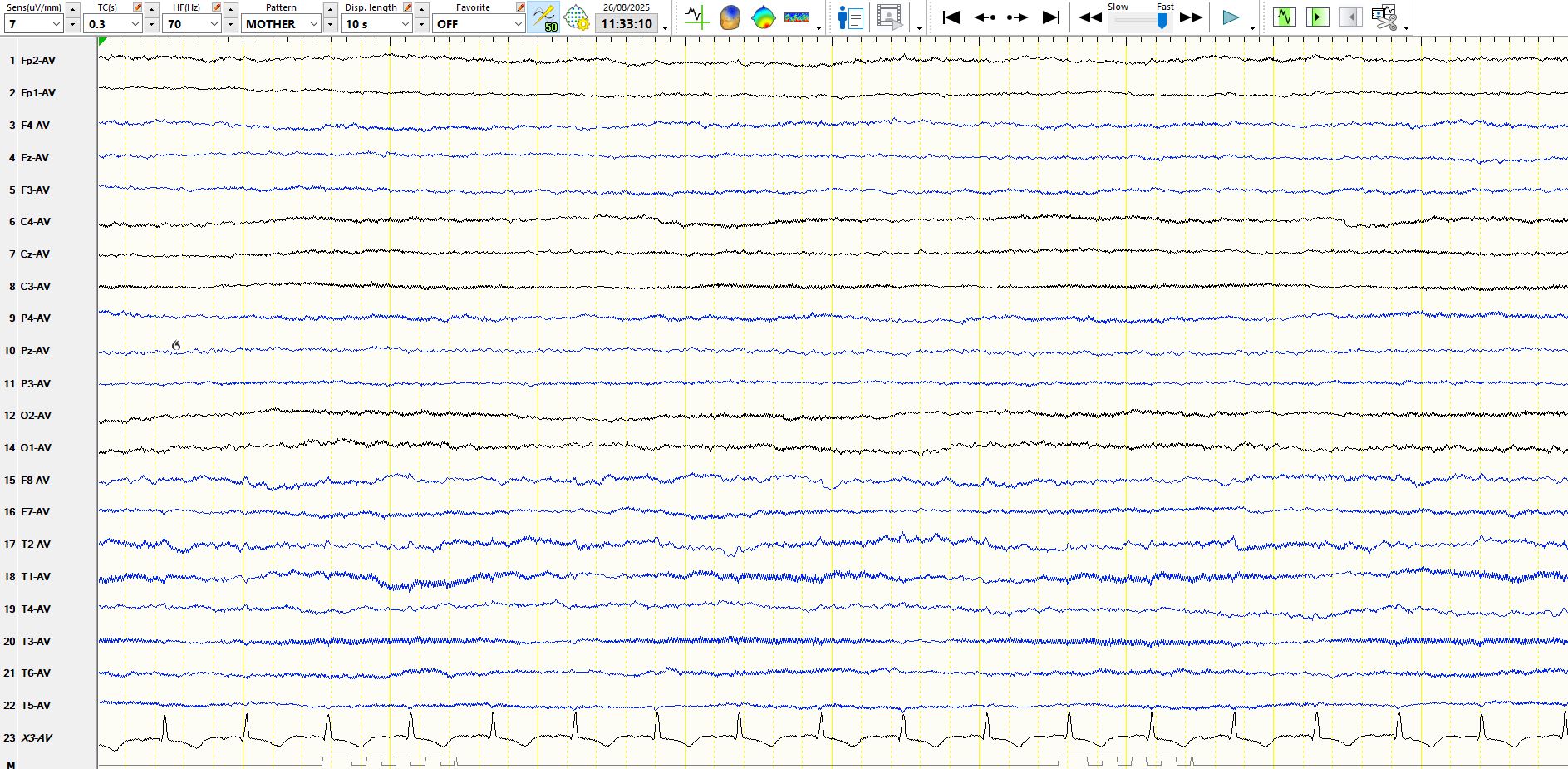
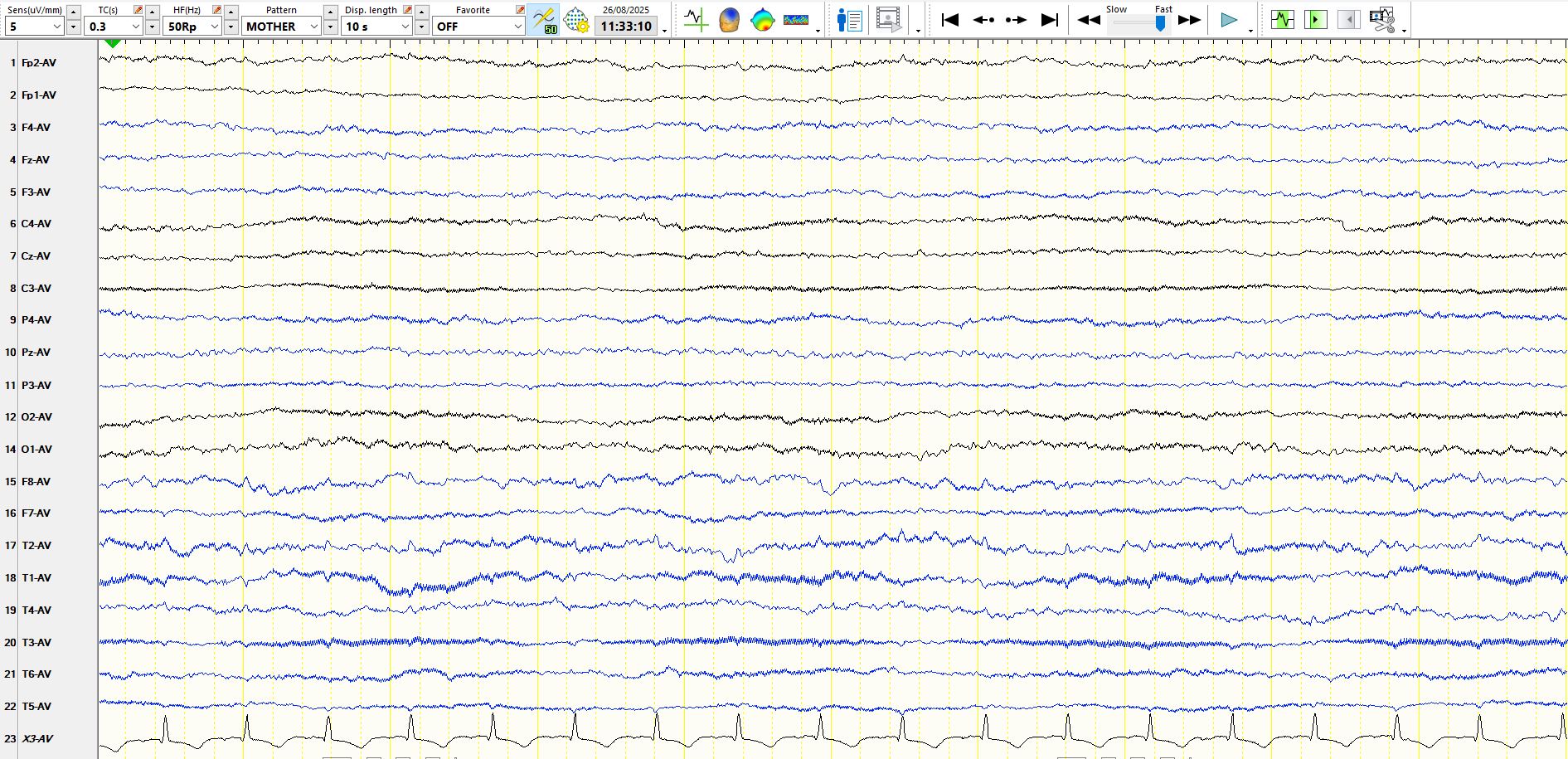
Figure 4. referential montage, 7 µV per millimetre:
Figure 5. Referential montage, 5 µV per millimetre:
These can be quite tricky because of environmental artefact in the ICU. However, be very careful of filters, other than the notch filter. Filters can easily convert environmental artefact into waves that resemble cortical rhythms. In figure 1, I cannot see any definite cortical rhythms. When one makes this judgement, you should be looking out for waves that are physiological or pathological but of cortical origin. There are multiple electrode artefacts, including at F8, M2 and T4. The latter artefacts produce "pseudo-cortical rhythms" in the same derivations, but these stand in stark contrast to faster frequencies in the alpha and beta range in other electrodes. Hence, it is highly unlikely that this area of cortex is reasonably functional, while the rest of the brain is not, doubly so because there are significant artefacts at F8 and T4. Similar conclusions pertain to figure 2 and, where the waves are represented on the coronal montage at 7 µV per millimetre respectively. Perhaps most strikingly, on the common average montage, where widely synchronous electrode artifacts may contaminate the reference, there is clear evidence of suppression of background rhythms.
You might therefore report the EEG as follows: "The EEG demonstrates no cortical rhythms ("electrocerebral inactivity") at 7 uV per millimetre, indicative of a severe generalised encephalopathy. Reversibility should be decided clinically". In the report it is best to avoid judgements about brain death and prognosis, which are substantially based on clinical data. It will also force the clinician to think carefully about reversible factors (hypothyroidism and hyperthermia). In this instance the clinician mentioned that the patient had not been given CNS acting medications for the past 36 hours. Even this requires care as some medications, such as the barbiturates, may have prolonged effects on the EEG and the level of consciousness. Ideally, the technologist should tap on the electrodes to ensure that they are working and assess responsiveness by stimulating the patient. Repeat EEG recordings are often a good idea, as continued suppression on EEG provides reassurance that the observation is correct and that in the intervening period there has been no change or reversibility.