Electrode artifact versus spikes in 1 electrode
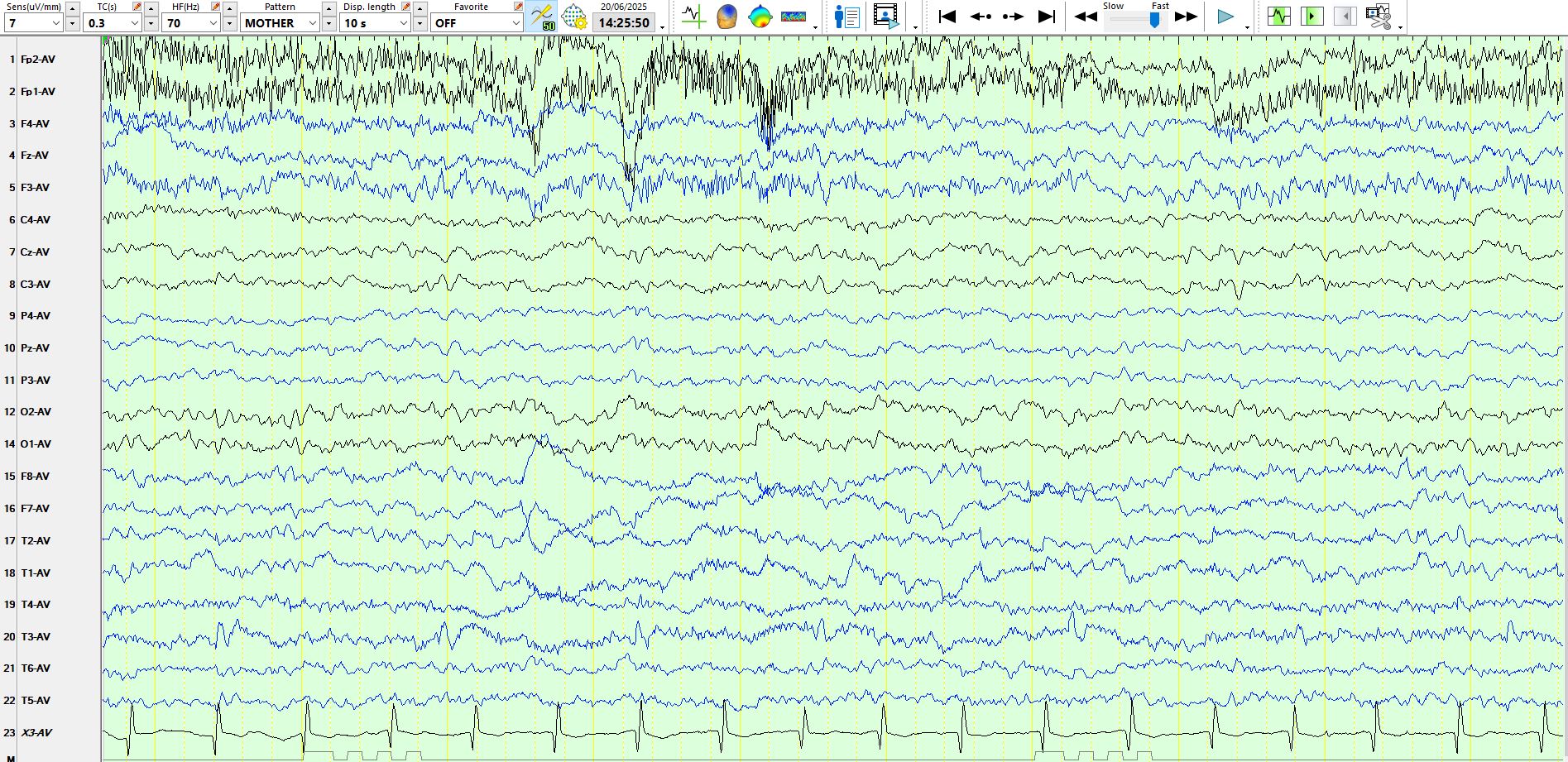
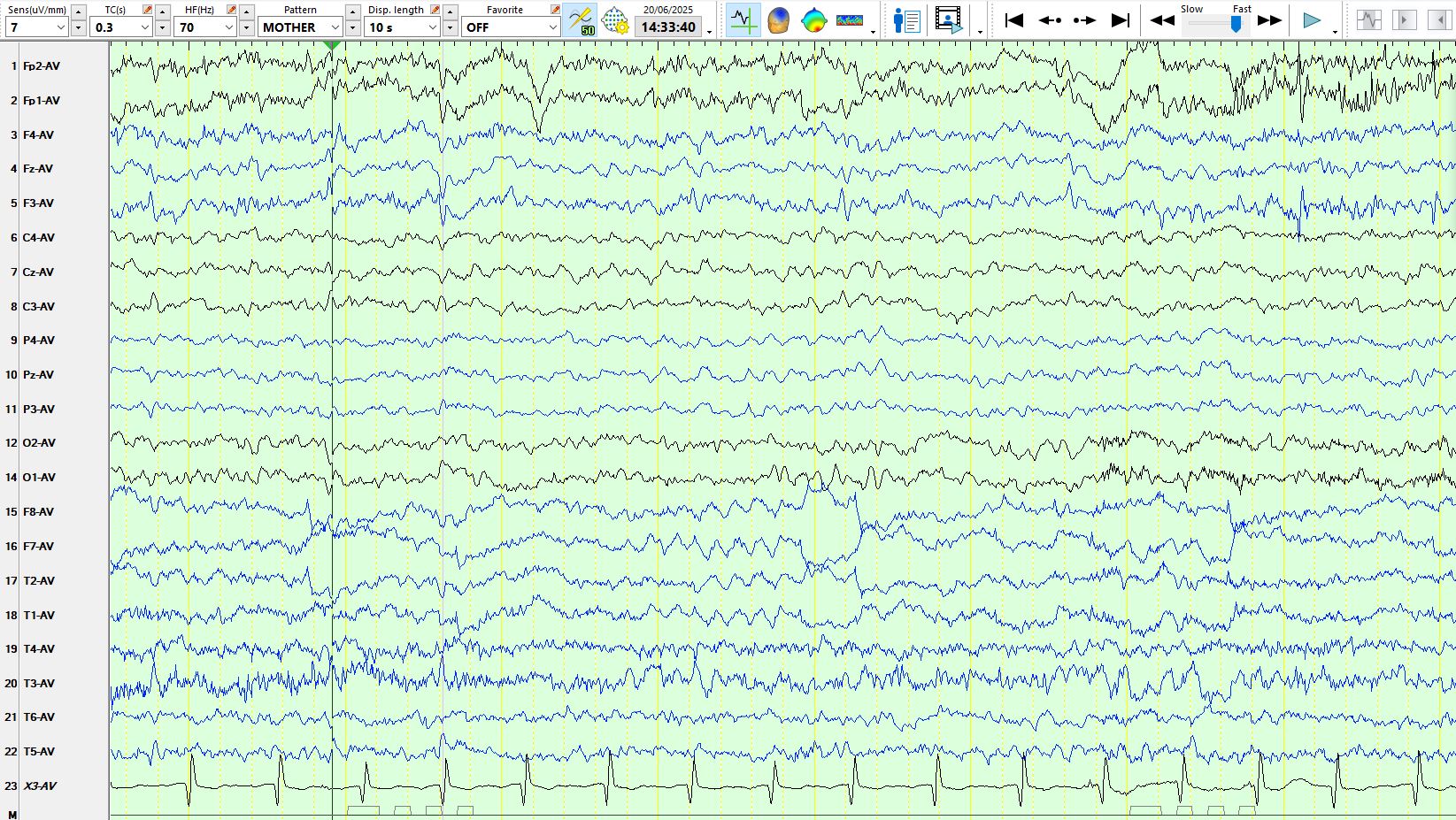
Jun 21, 2025One can certainly see spikes in one electrode. However, this is an uncommon phenomenon and more often than not a sharply-contoured wave or a spike-and-wave-like discharge is an electrode artifact. Have a look at the following page of a five-year-old referred to a paediatric neurologist because the occupational therapist witnessed brief blank staring episodes, lasting no more than a few seconds. The parents have never witnessed any episodic neurological events, including on systematic enquiry (I went through this carefully with the mother). What do you make of these waves at T3?
While some of them are coincident with ECG beats, others are not, and these do therefore not represent ECG artefact. Each of these is followed by a slow wave. Adjacent electrodes (T5, M1, F7, C3) are not obviously involved. Still, one has to be very cautious, especially on a referential montage. Hence, always have a look at it on another montage:
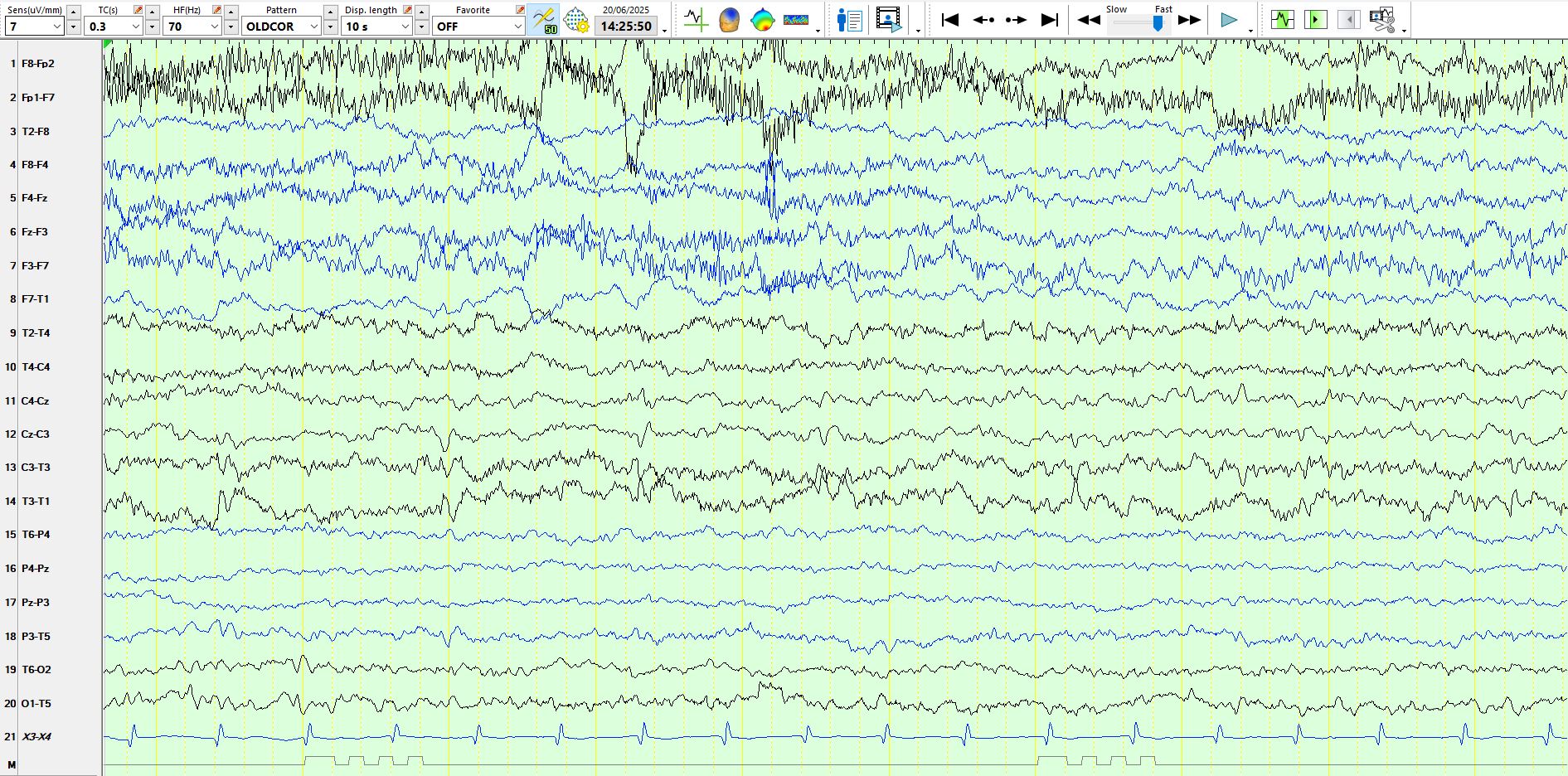
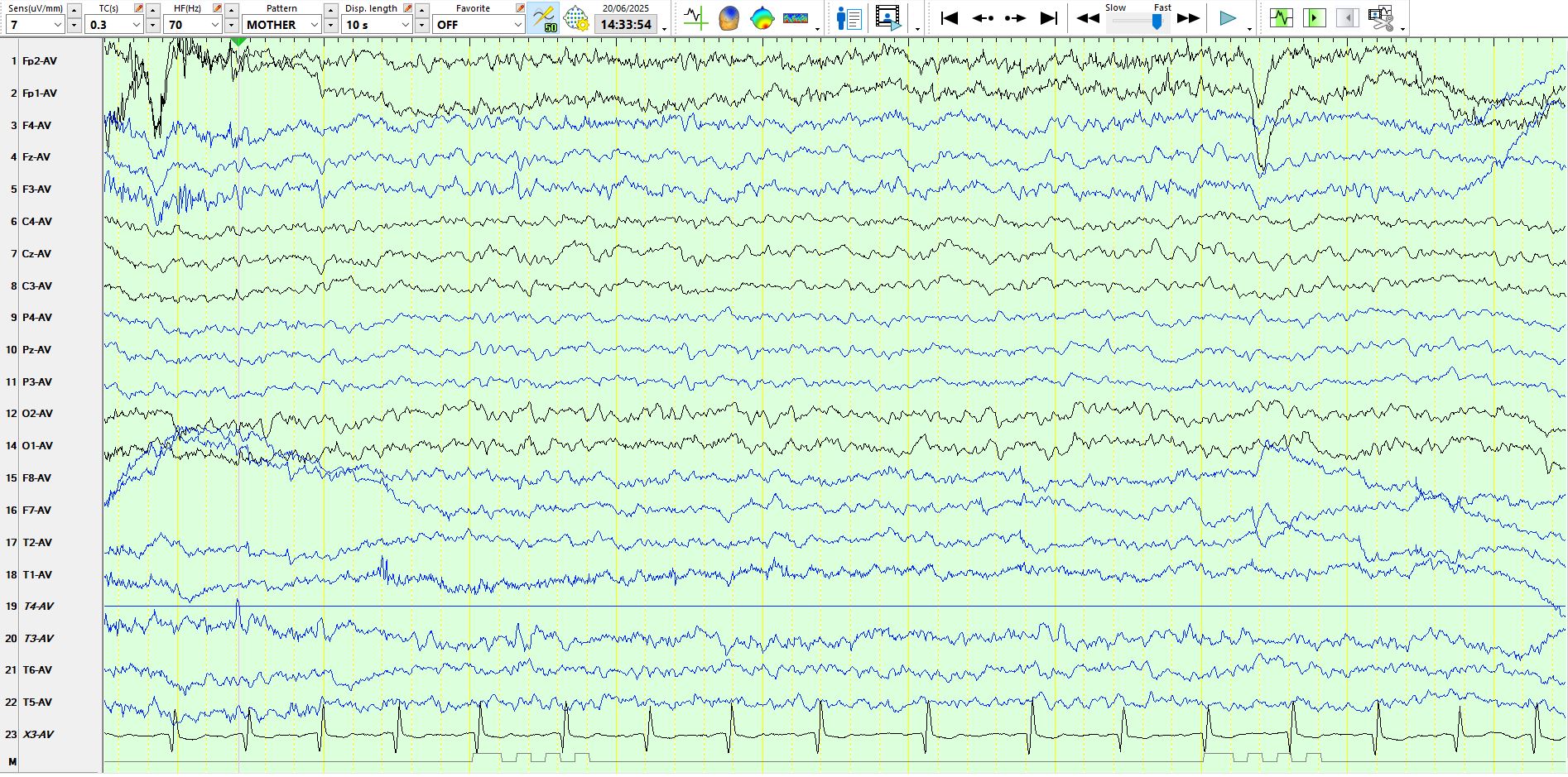
The coronal montage above provides unambiguous evidence for a typical field for both the spikes and the slow waves seen on the top image and, while there is a partial electrode artifact at T3, this does not explain the spike-and-wave-like discharges. Hence, these represent definite spike-and-wave discharges at T3-C3. If you revert to the top image, you will notice very subtle involvement of C3.
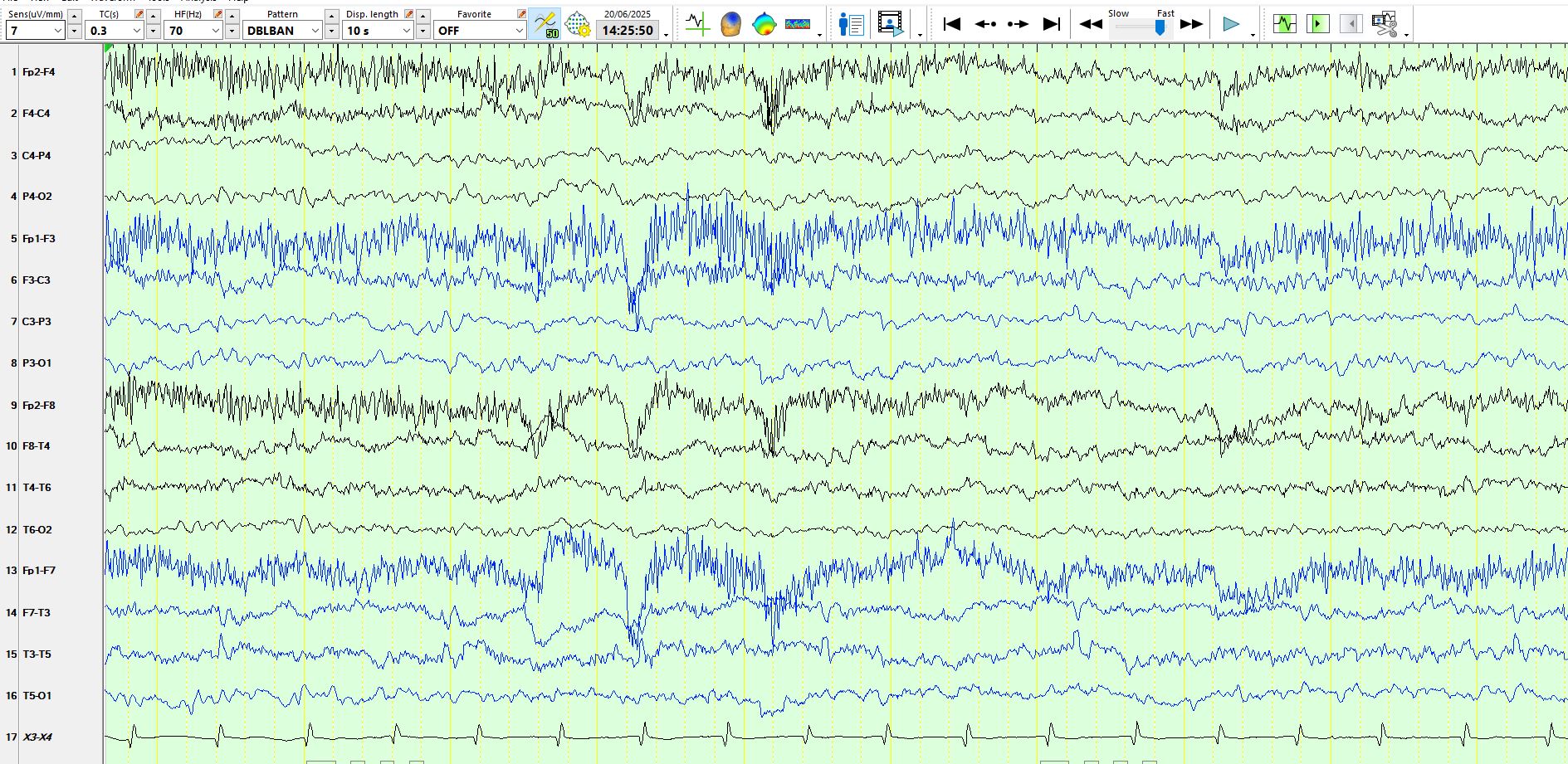
You will come to similar conclusions having looked at the same page on the bipolar AP montage (see the image above).
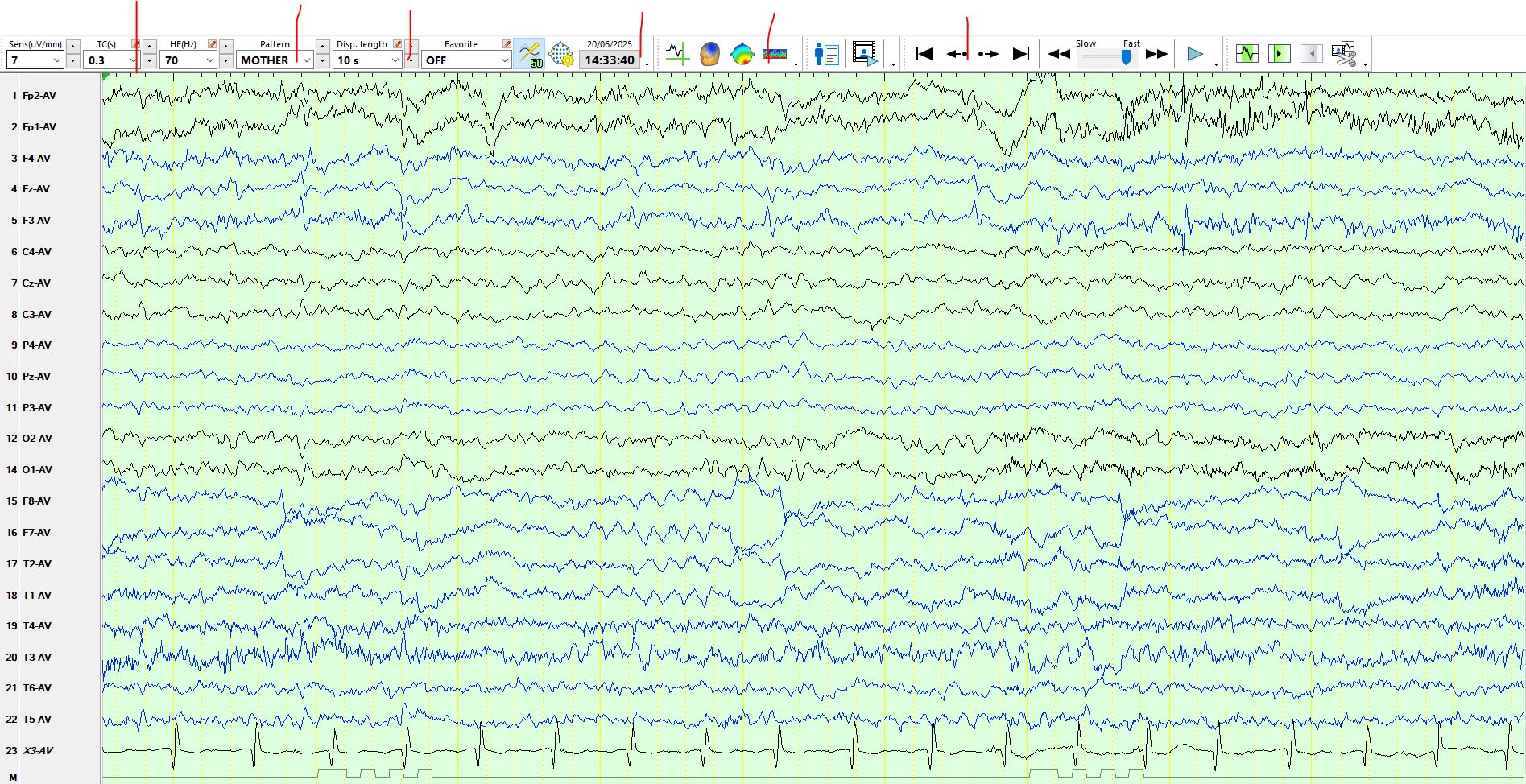
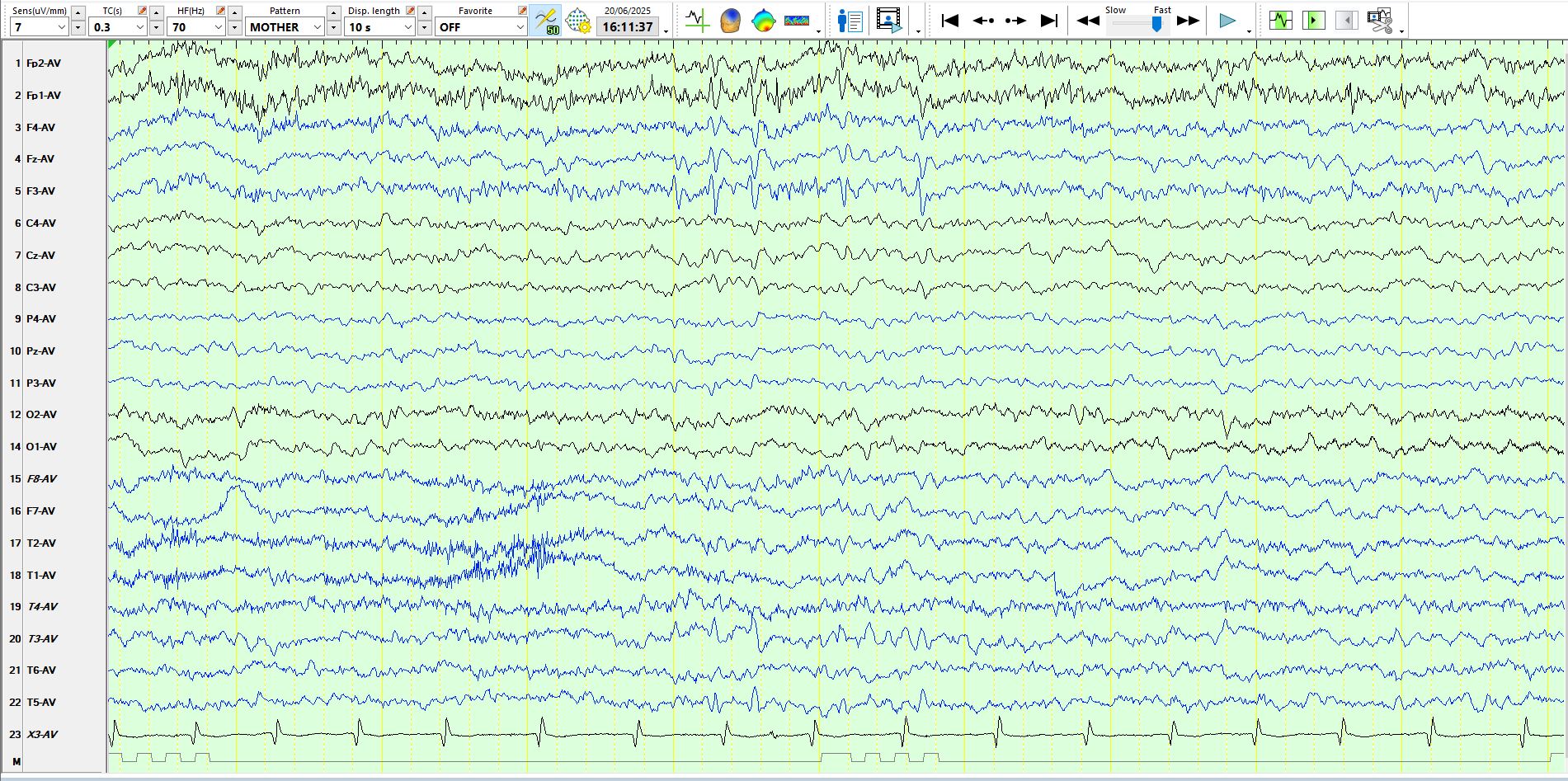
Scroll on a bit further and you come across the following page. Does the patient also have left frontal spikes (F3) and would you therefore conclude that the patient has multifocal spikes? Have a look beneath the six vertical red lines on the image below.
You will notice that the six highlighted waves at F3 above have a very similar shape, but there is a subtle variation in the shape of these. This is common with spikes; the reason for this is a discussion for another day. The above waves are biphasic, indicating that the first component is surface electro-negative and the second phase is surface electro-positive at F3. Now, if you look at these waves, especially obvious with the third one, notice that the electro-negative phase is synchronous with an electro-positive component in the electrodes immediately adjacent to F3, including FP1, FZ, F4, FP2, Cz, C4, indicating a dipole. If you look carefully at the third of these highlighted waves, you will see that T3 also shows an "upward" deflection at this time. This bears further scrutiny, especially as F3 and T3 are not exactly close neighbours.
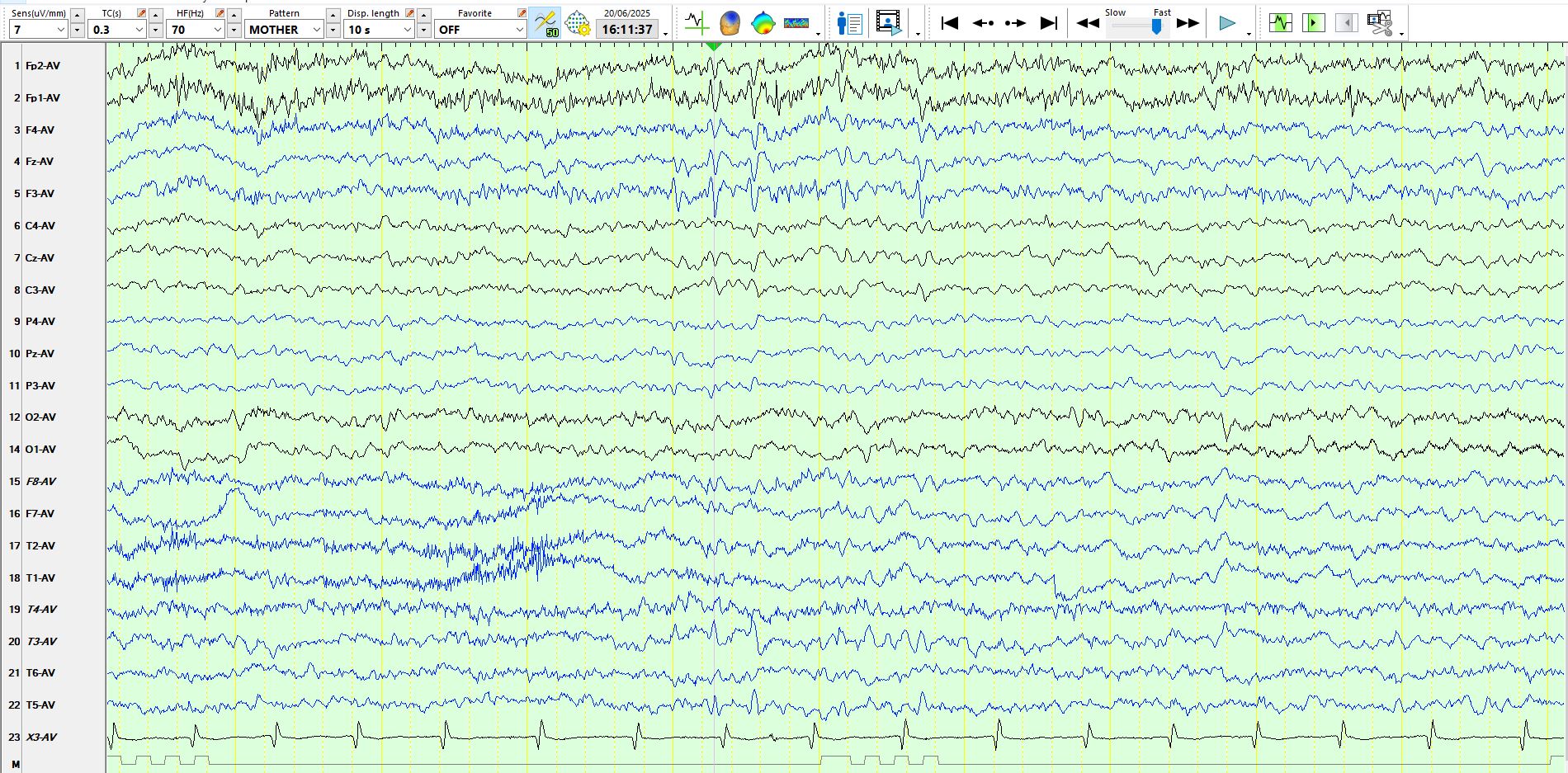
With the time analysis function (the vertical lines above) switched on, you can see that the waves at F3 are not precisely coincident with those at C3 and T3. When the wave is electro-negative at T3-C3 it is either electropositive or equi-potential at F3, providing further evidence for the dipole, especially as C3 and F3 are neighbours.
This oblique dipole, its morphology and the absence of focal delta waves or theta waves in the same region is highly characteristic of Benign Rolandic Epilepsy of Childhood (also known as Benign Epilepsy with Centro-Temporal Spikes (BECTS). The current term for this form of epilepsy is "self-limited epilepsy with centrotemporal spikes". Recognising the key electrophysiological features is crucial in arriving at the diagnosis. Does this child have epilepsy? This again ends up in one of those silly arguments about the definition of epilepsy. This child likely has the genes responsible for this form of epilepsy. Because these seizures may occur in sleep only or largely in sleep, these may simply have gone unnoticed. You can see the point about the futility of the argument about the diagnosis of epilepsy. Of course, one should not treat an individual with antiseizure medication unless there are clearly identifiable epileptic seizures or definite cognitive consequences of seizures (occasional patients may have electrical status epilepticus in sleep, without clinical seizures). These discharges simply mean that the patient is predisposed to the development of epileptic seizures and likely carries the genes described above. What did the occupational therapist notice? Perhaps these were brief dysphasic episodes, representing brief focal seizures. Equally, they may have been episodes of daydreaming/inattention, which I fancy is the more likely, since the parents have never seen anything. Such periods of daydreaming are more likely on the day following a clinically unrecognised seizure during sleep, as the sleep architecture would have been disrupted and fatigue following focal seizures may last days. Trials of therapy are generally a very bad idea, doubly so when you do not have a measurable outcome.
PS: your initial instincts were incorrect: the patient does not have multifocal spikes.
Dipole tracing in childhood epilepsy with special reference to rolandic epilepsy - PubMed
Benign rolandic epilepsy of childhood: topographic EEG analysis - PubMed
There is another example below. The trains of spikes raise another possibility; perhaps the episodes of fleeting "staring and zoning out" are a consequence of these.

Here is another:
And here is another example
The following is the same page as above, but with the time analysis activated.