65y, two episodes of amnesia
May 12, 2025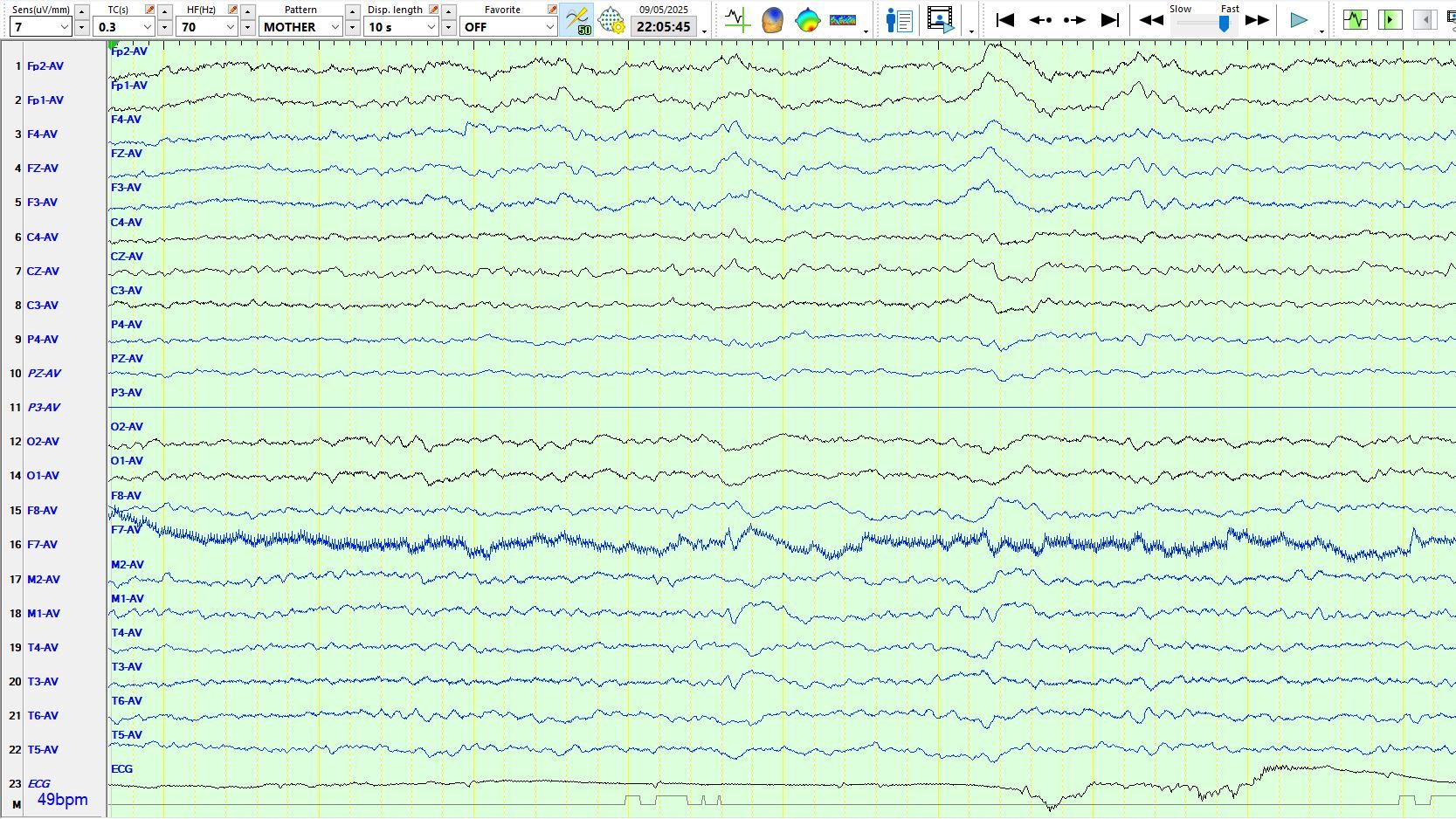
65y, two episodes of amnesia lasting 1.5 hours and about three hours, previous traumatic brain injury with amnesia for approximately 24 hours
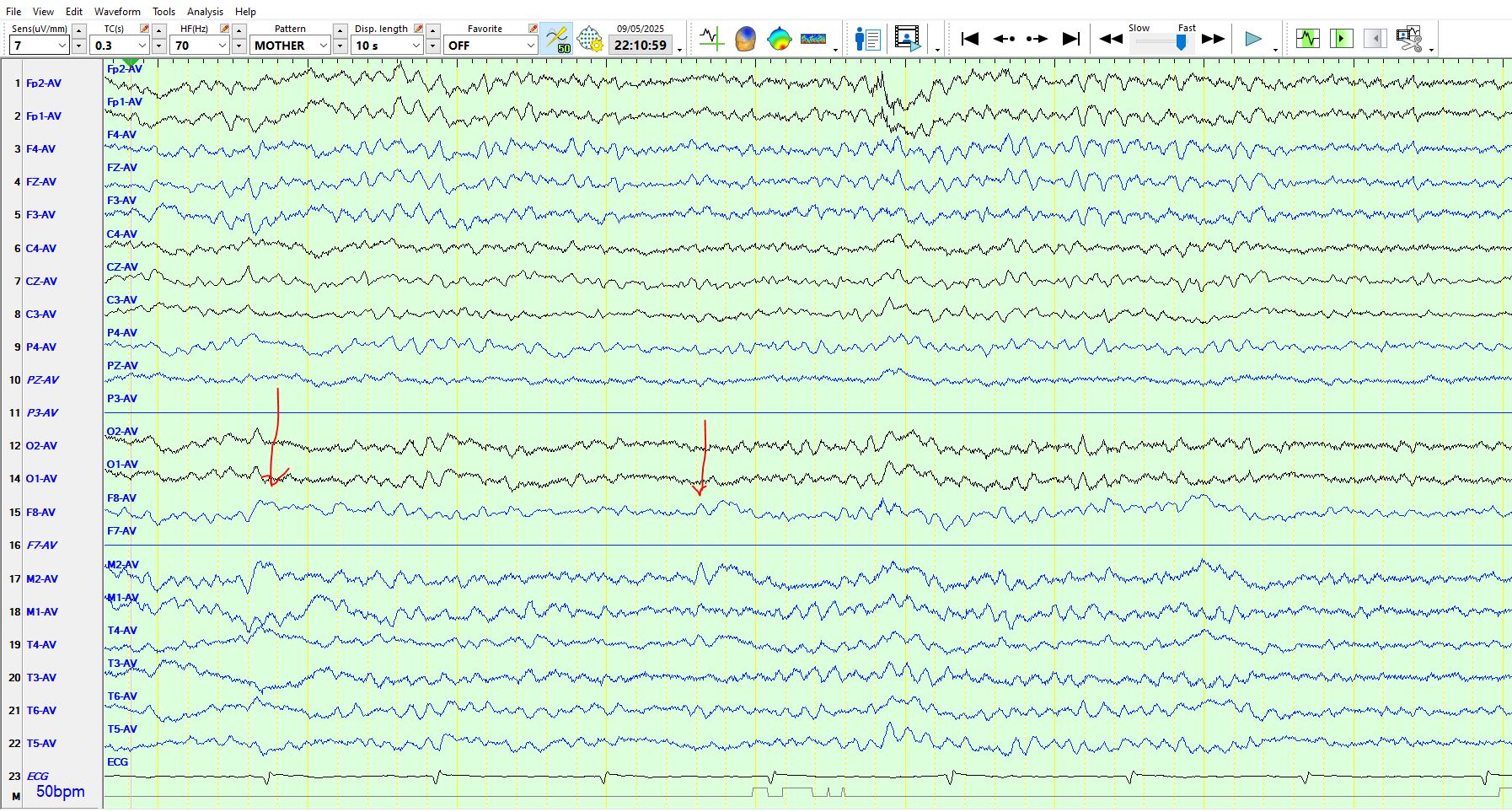
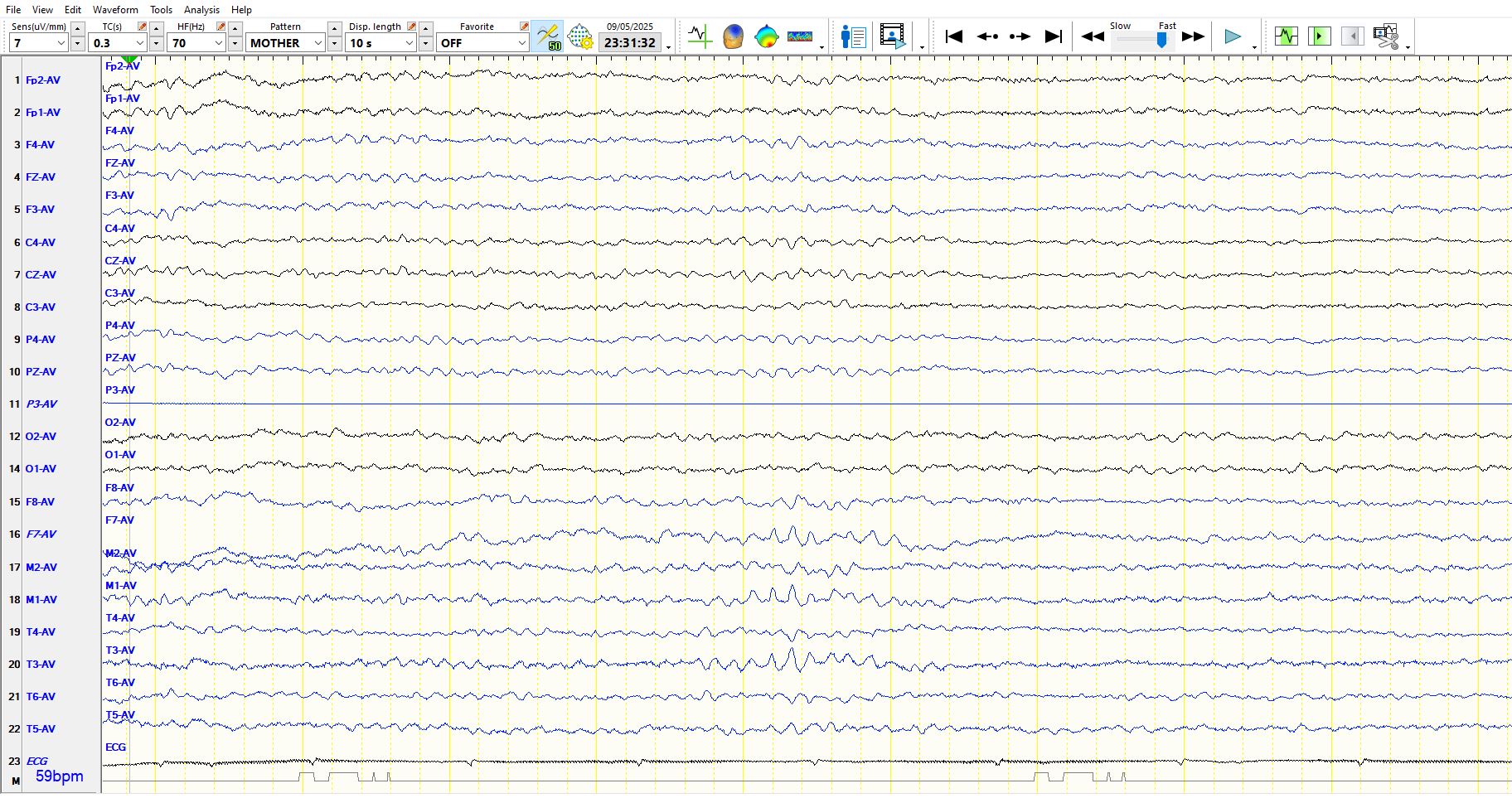
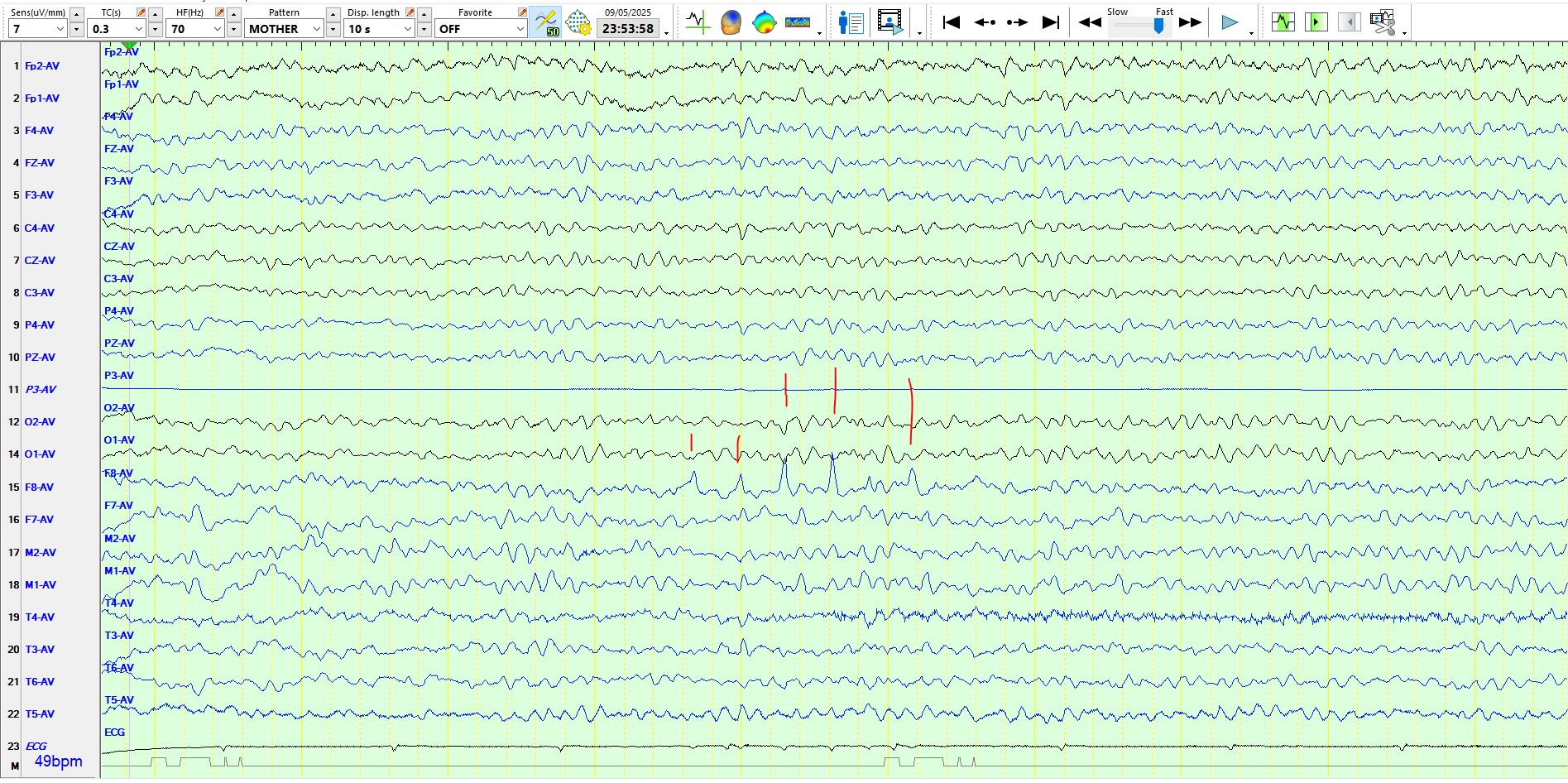
F7 is artifactual, but only partially so and the representation of the waveform seen at M1 and T3 is similar, providing assurance that this slow wave and the preceding sharper wave is of cortical origin in F7. The waveform is therefore represented at F7-M1-T3. Is the sharper component of the waveform sufficient to call this a spike-and-wave discharge? There should be great caution in calling this a spike-and-wave as the sharper component may simply be part of the background rhythms in the same channels. Hence, it is necessary to
1. Review the background rhythms extensively, in this case during stage II sleep, before deciding about calling this a spike-and-wave discharge.
2. Sometimes it is useful to move the screen so that the delta wave disappears off the screen on the right, while the sharper component can still be seen. Notice the arrow on the right-hand side of the screen below; the "sharp wave" appears completely innocuous and is not a sharp wave!
3. Turn off the artifactual channel, which may amplify or distort the appearance of the sharper component and trick you into believing that the waveform is a spike (see the page above, arrow on the right)
4. Looking elsewhere in the recording for waveforms that may be called spike-and-wave; if there is no other waveform elsewhere in sleep that can convincingly be called a spike-and-wave discharge, it would be prudent to err on the side of being conservative. As is the case in science generally, look for reproducibility.
5. Always check that the sharp wave is not a QRS complex (ECG); in this case it is not.
If there is any doubt, call this an abnormal delta wave over the left anterior, inferior temporal region, while avoiding the possibility of over-calling this as an IED and inadvertently resulting in an incorrect, enduring diagnosis of epilepsy for this patient. Remember, by over-calling anything that is remotely doubtful, the EEG loses its specificity and therefore predictive value for the diagnosis of epilepsy. Normal variants and artifacts: Importance in EEG interpretation - PubMed
Just for good measure, notice that there is a similar delta wave at M2-F8-T4 (the right inferior, anterior temporal region) during sleep, preceded by a sharper wave that is indistinguishable from the preceding and succeeding background rhythms. Notice also the abnormal theta wave at M2-F8-T4 (the arrow on the left). In summary, none of the waveforms demonstrated here should be considered inter-ictal epileptiform discharges.
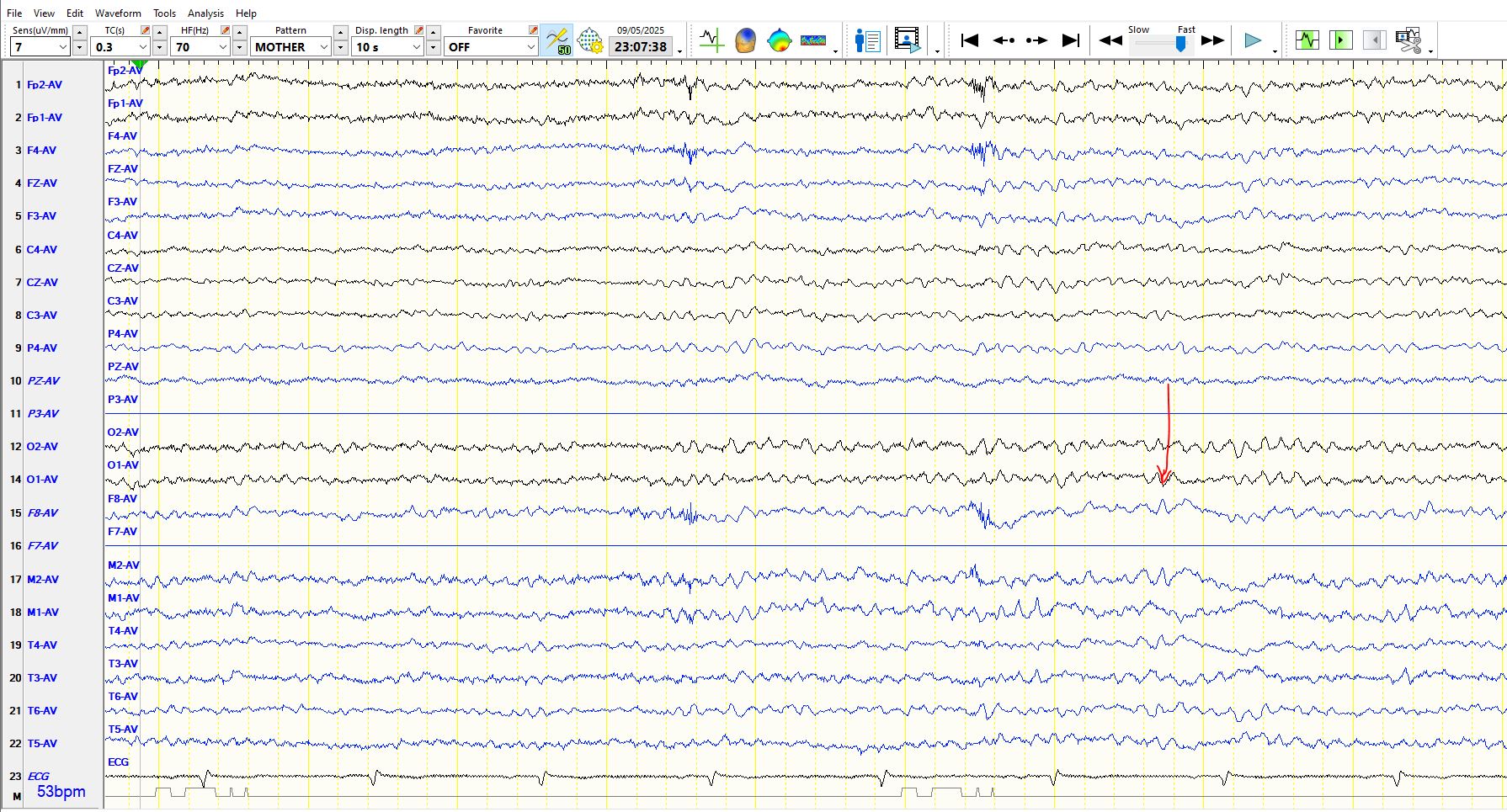
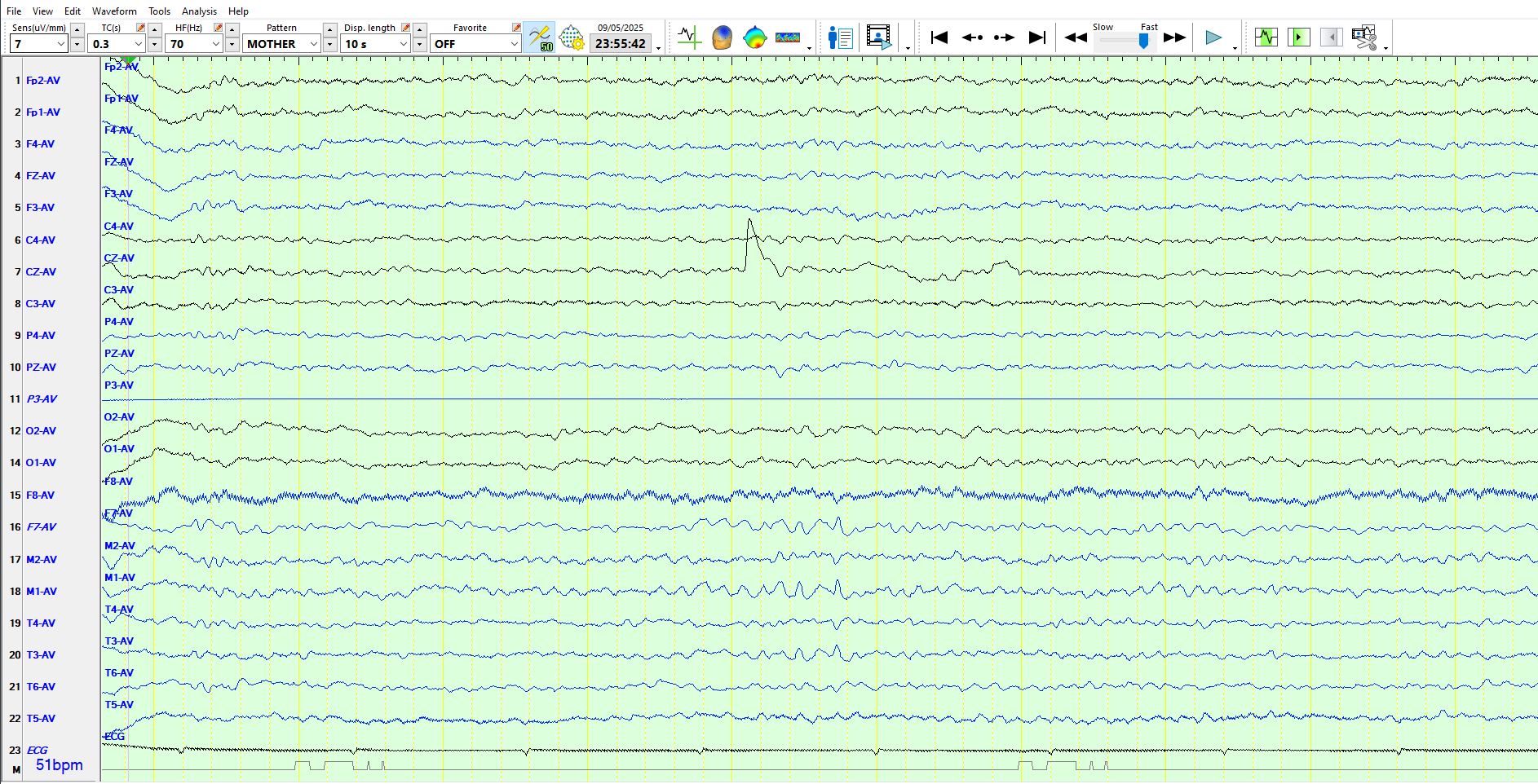
Here is another example of no more than a delta wave over the right inferior, anterior temporal region during wakefulness
And here is another
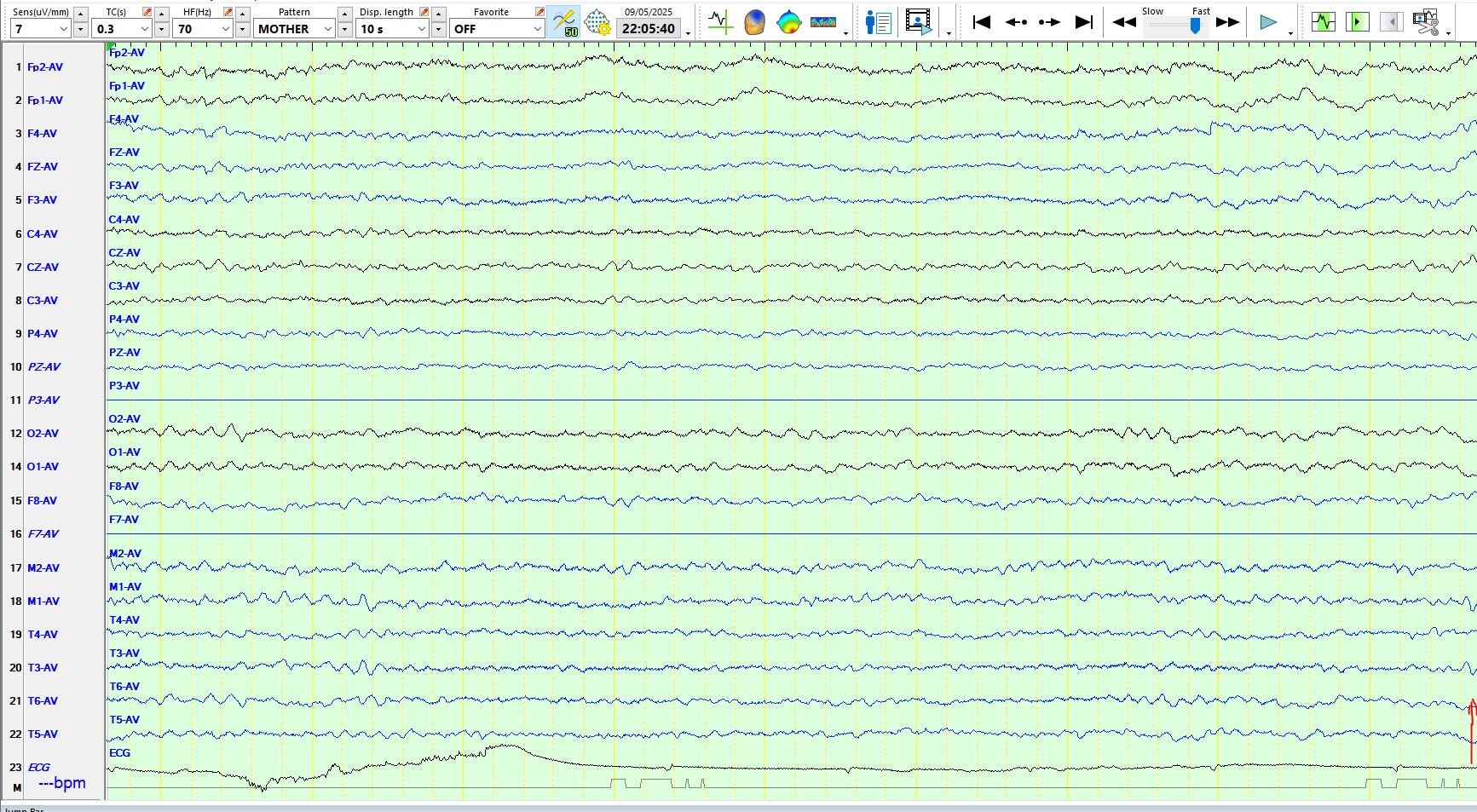
The following illustrates the waxing and waning nature of alpha in the temporal regions during drowsiness/stage I of sleep
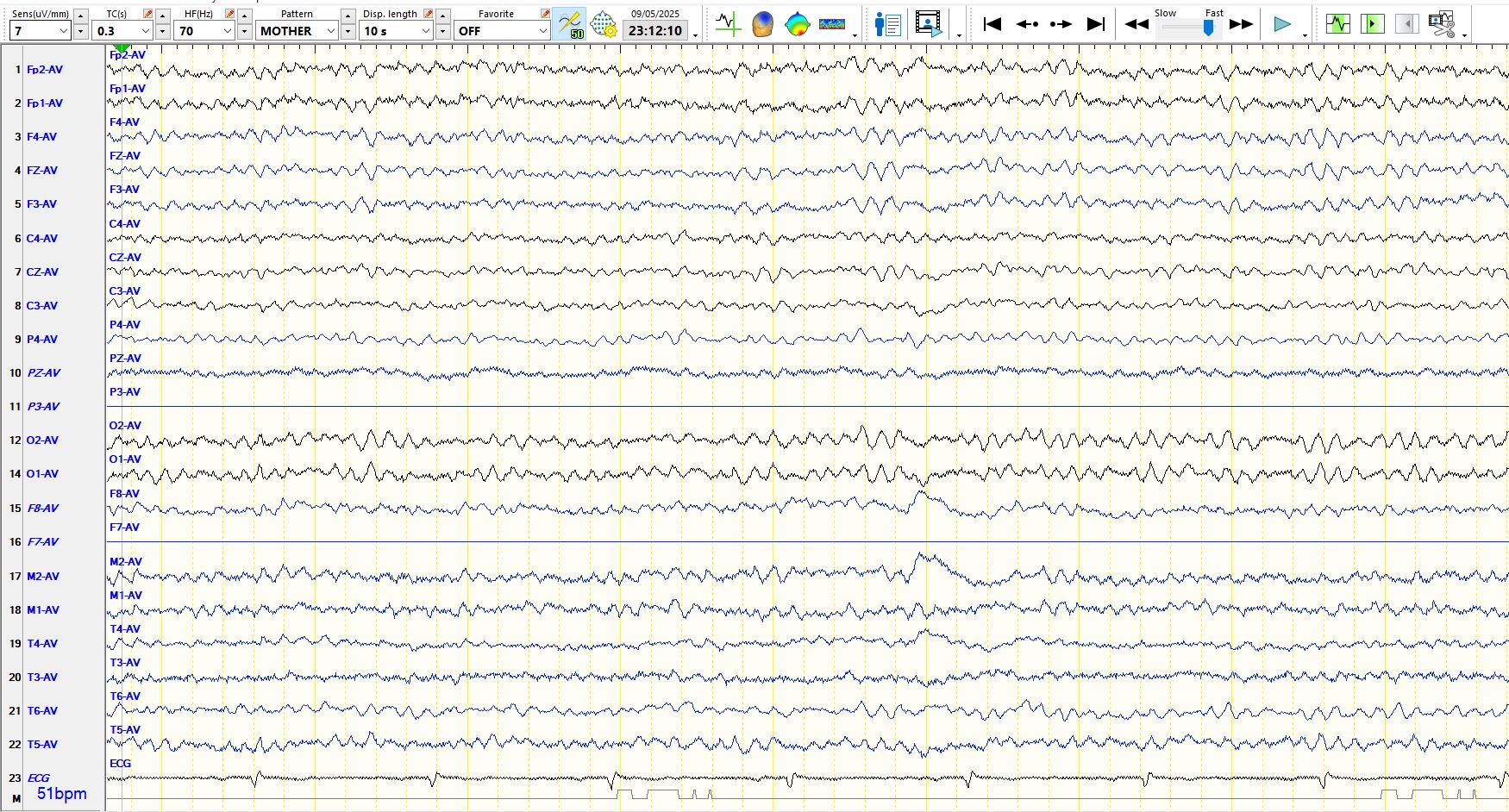
The following are not right temporal spikes either. The referential montage, including the common average, is particularly prone to represent artefacts in a way that resembles spikes. This is an F8 electrode artifact:
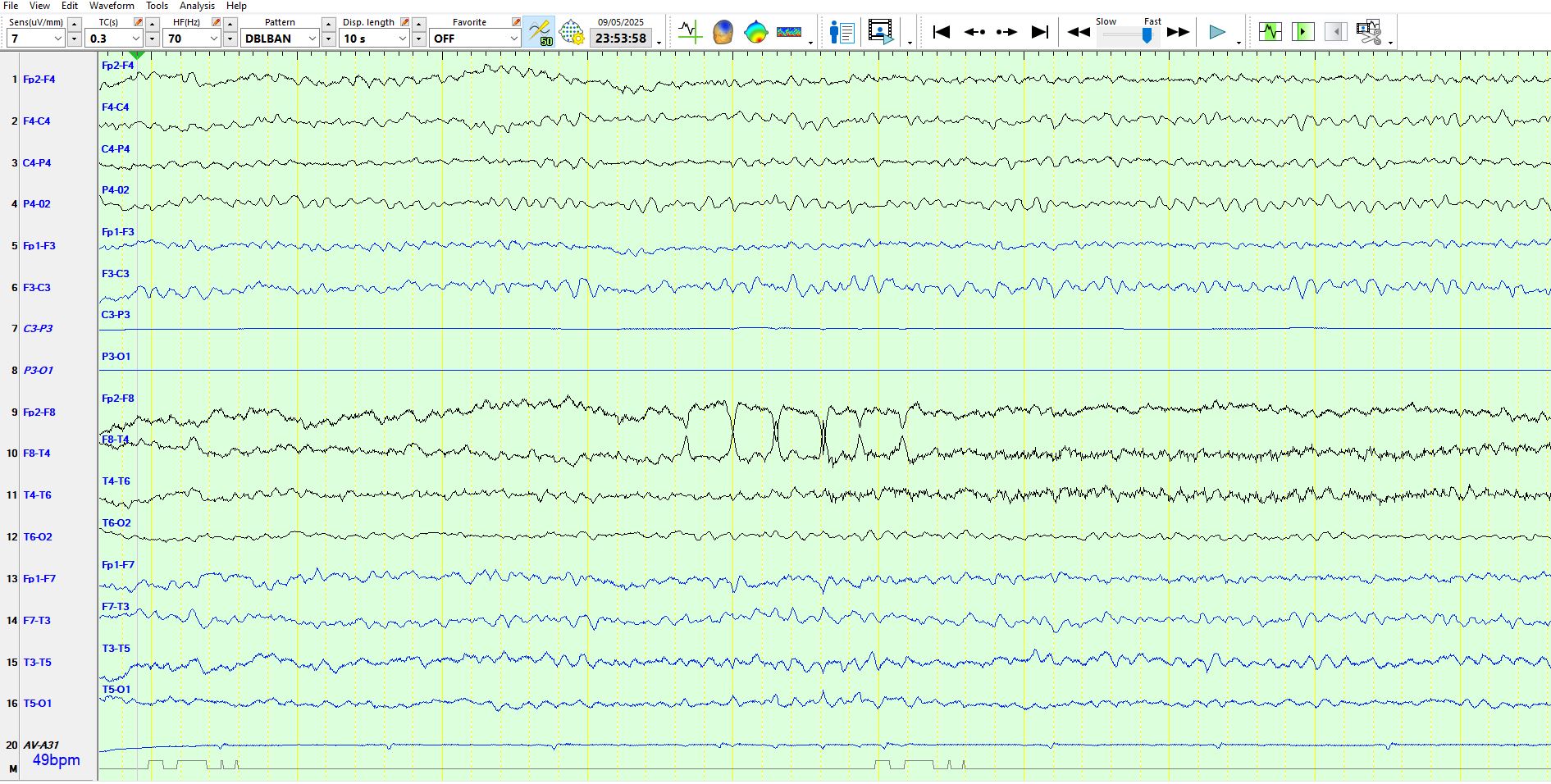
Here is the bipolar montage of the above 10 seconds:
Clinical interpretation
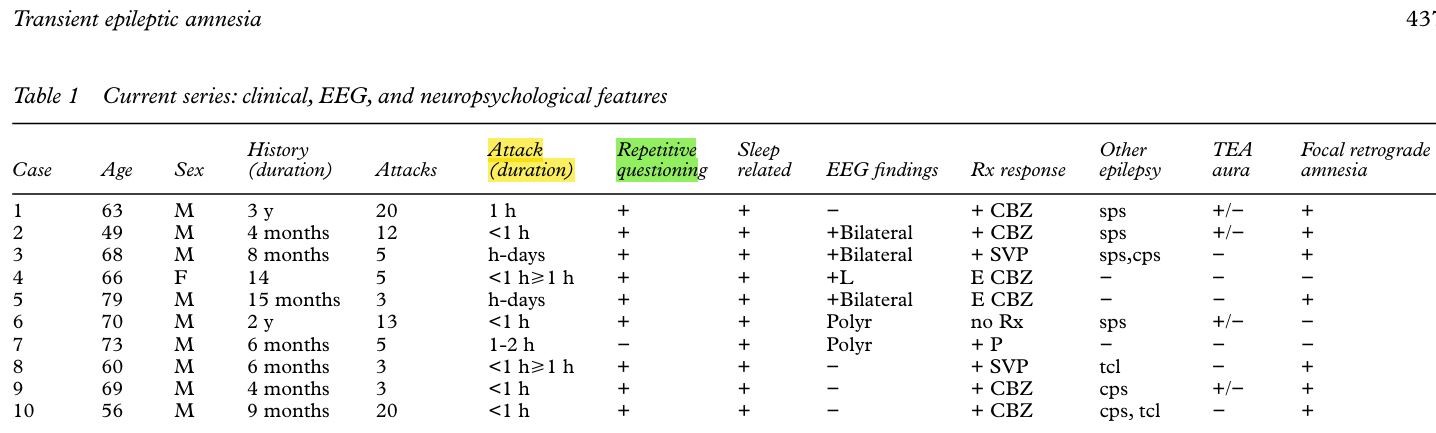
The EEG is abnormal, with non-epileptiform dysfunction over both inferior, anterior temporal regions. There are no inter-ictal epileptiform discharges. Hence, the EEG findings do not reliably distinguish between transient global amnesia and transient epileptic amnesia. The EEG is typically normal in someone with transient global amnesia. The non-epileptiform dysfunction most likely relates to the previous traumatic brain injury, the severity of which independently increases the likelihood of the patient developing epileptic seizures. Of note, while the two prolonged amnestic events occurred six months apart, the patient's behaviour and cognition appeared normal to his wife and he did not repeatedly ask questions, as is so characteristic of transient global amnesia. The duration of the events is typical of transient global amnesia, but long amnestic epileptic seizures, while relatively uncommon, may also result in prolonged amnesia, especially if the seizures involve both medial temporal lobes, are longer than usual and are followed by severe post-ictal hippocampal dysfunction (the equivalent of a Todd's paresis). In this instance, a confident distinction between the two possibilities cannot be made but, given his previous history of a traumatic brain injury, the interictal EEG findings and the absence of the typical questioning that occurs during transient global amnesia, transient epileptic amnesia is considered the more likely.
Transient epileptic amnesia: a description of the clinical and neuropsychological features in 10 cases and a review of the literature - PubMed