17, born prem, given O2, blind, MRI reported as normal
May 31, 2025...attends a school for blind people. What is the significance of the sharply-contoured waves?
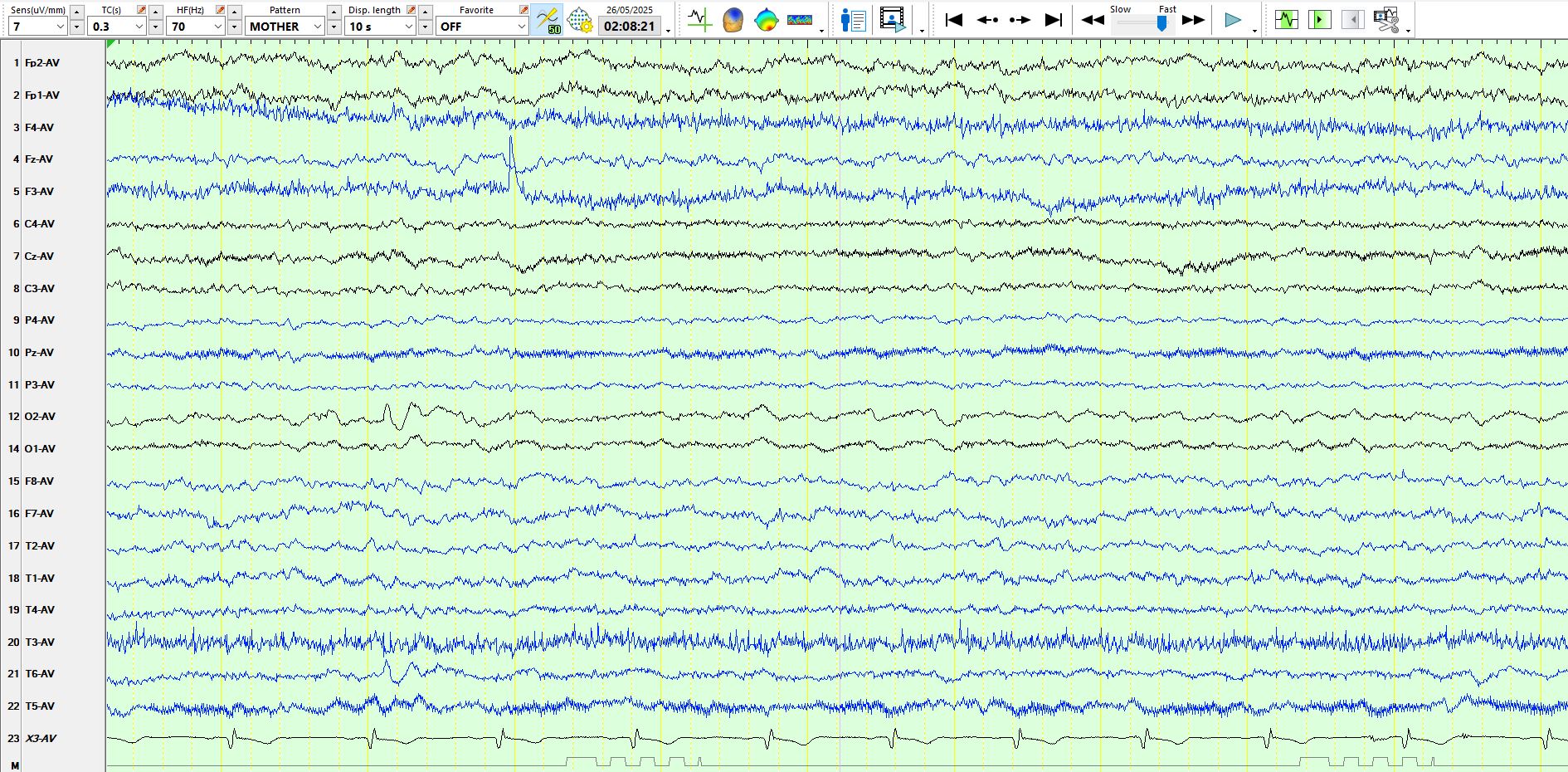
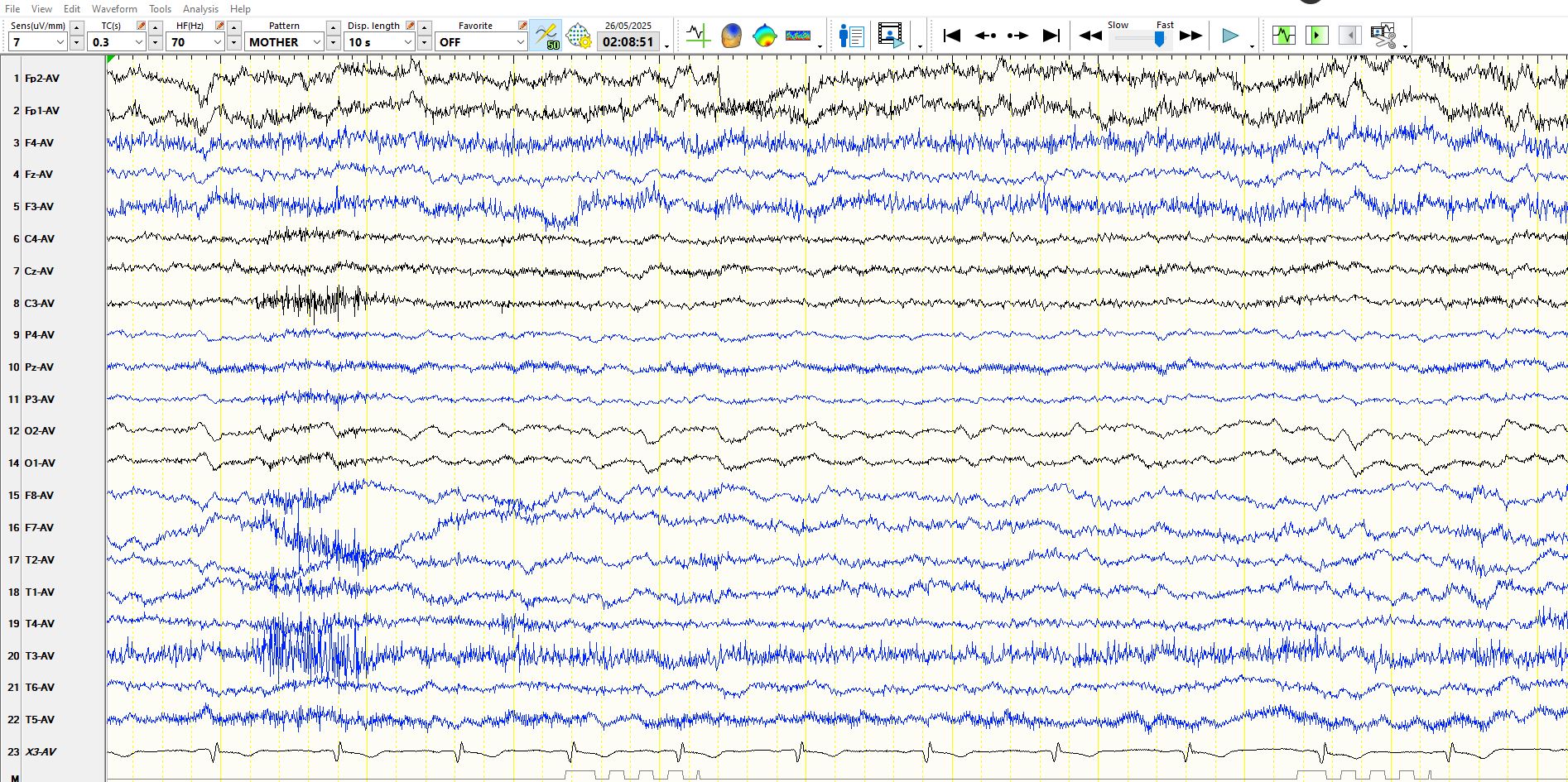
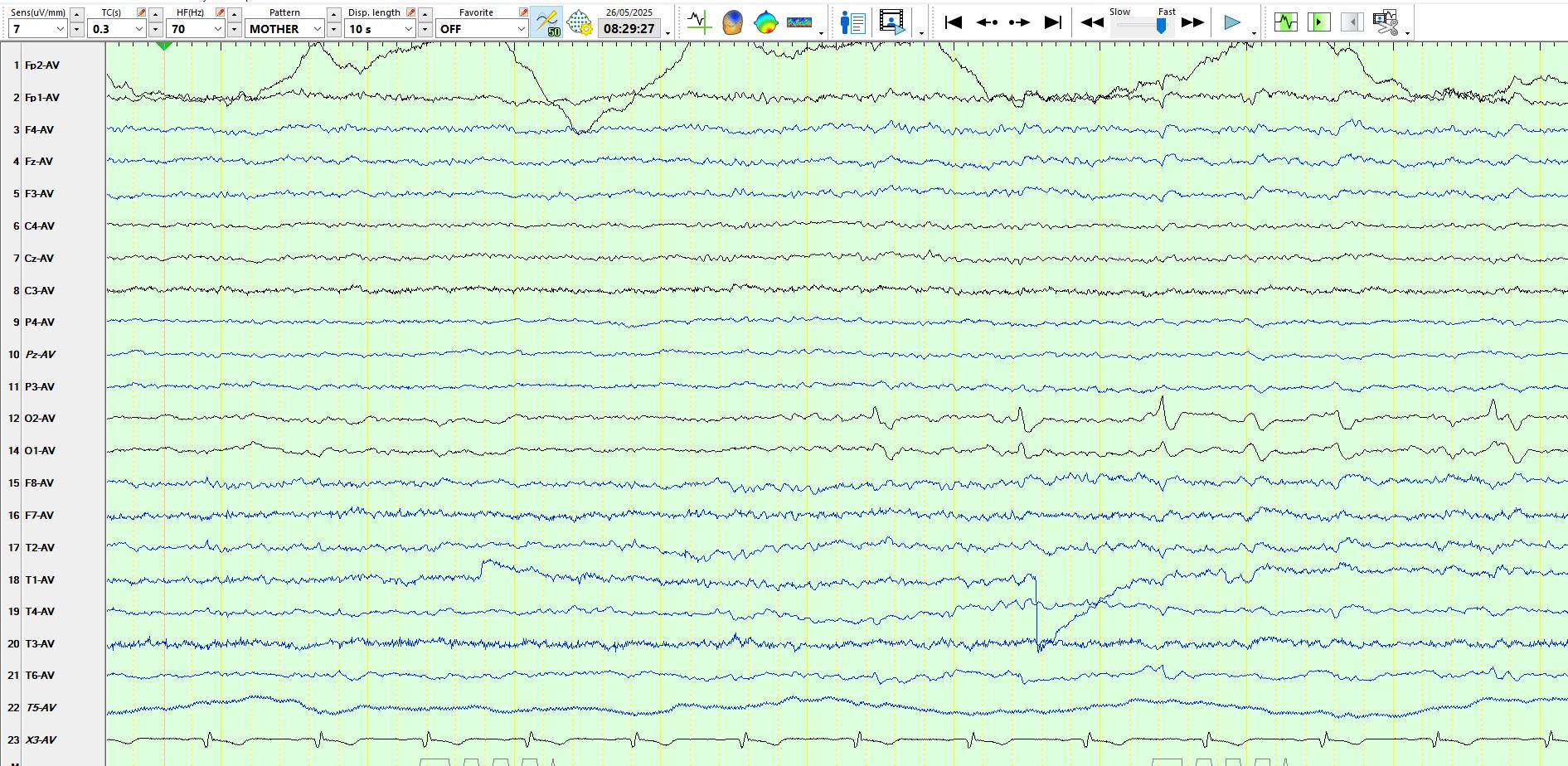
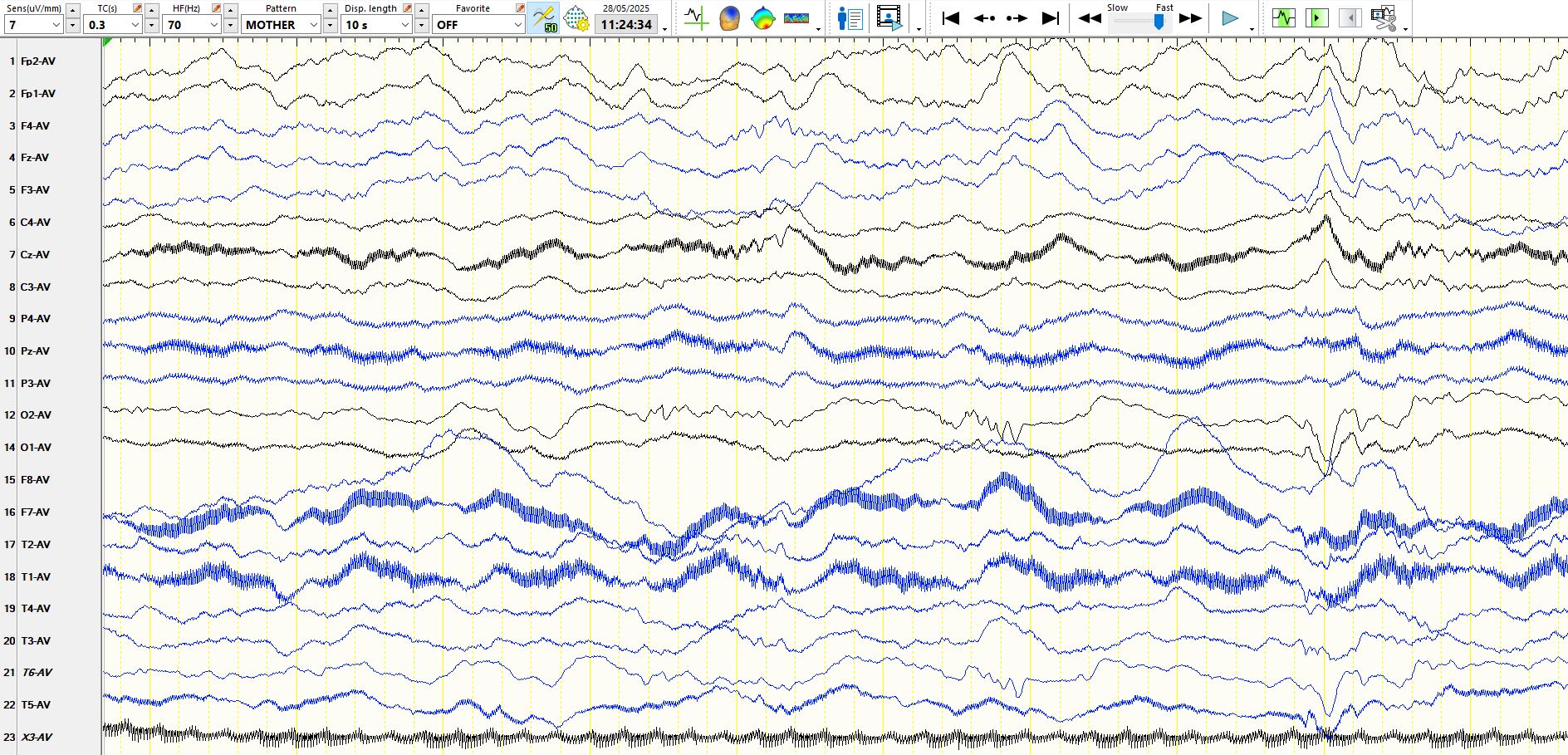
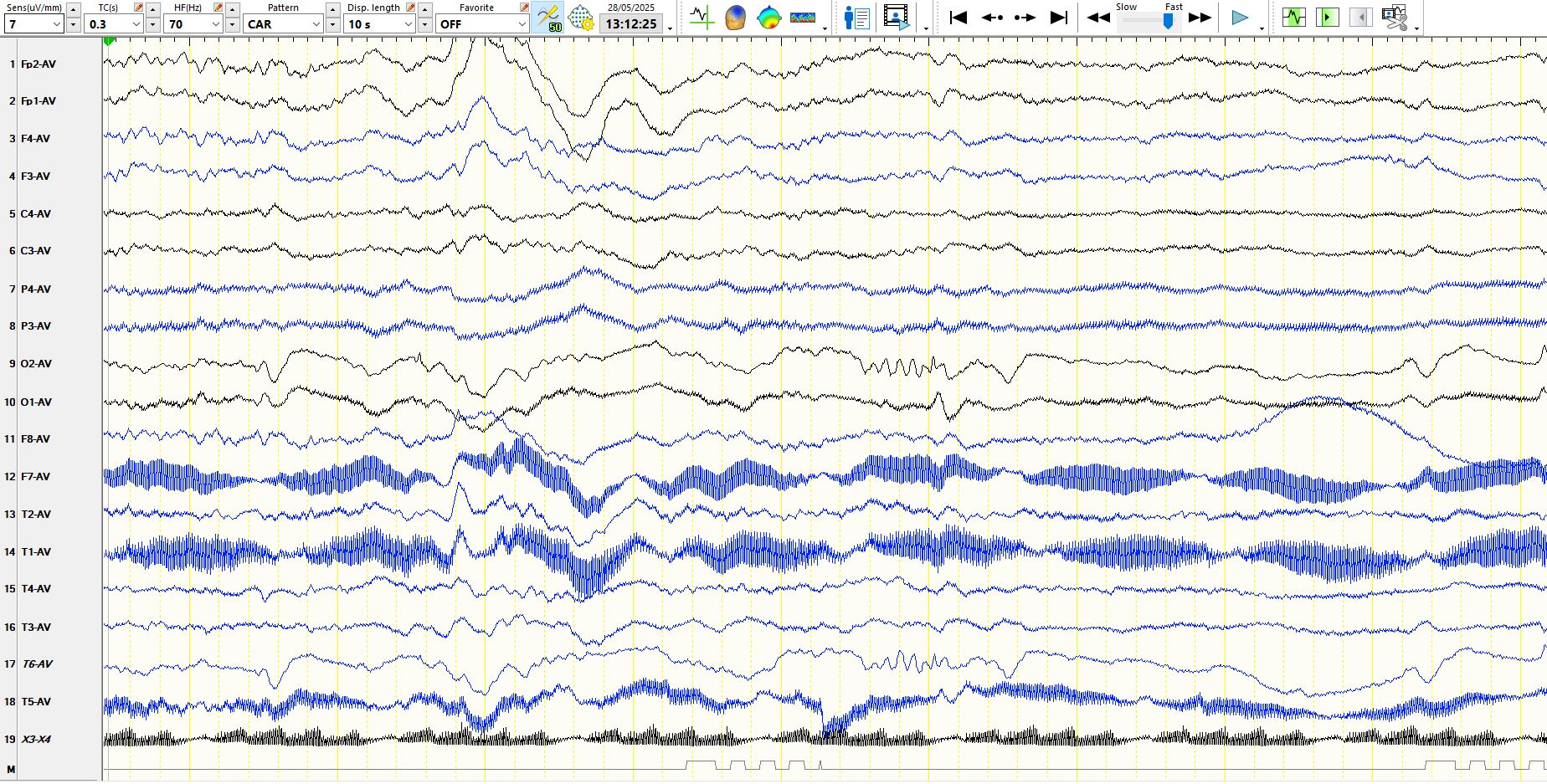
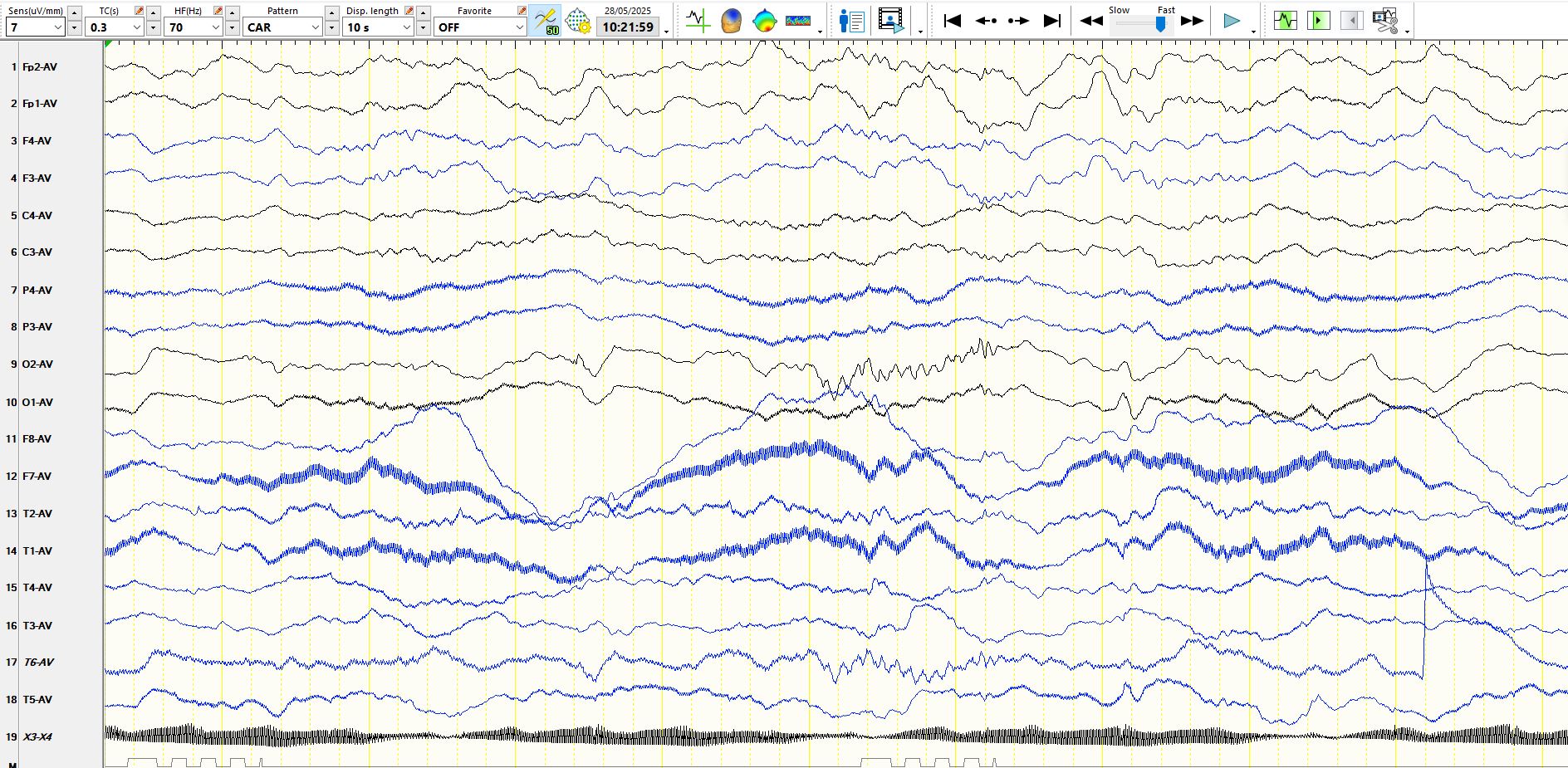
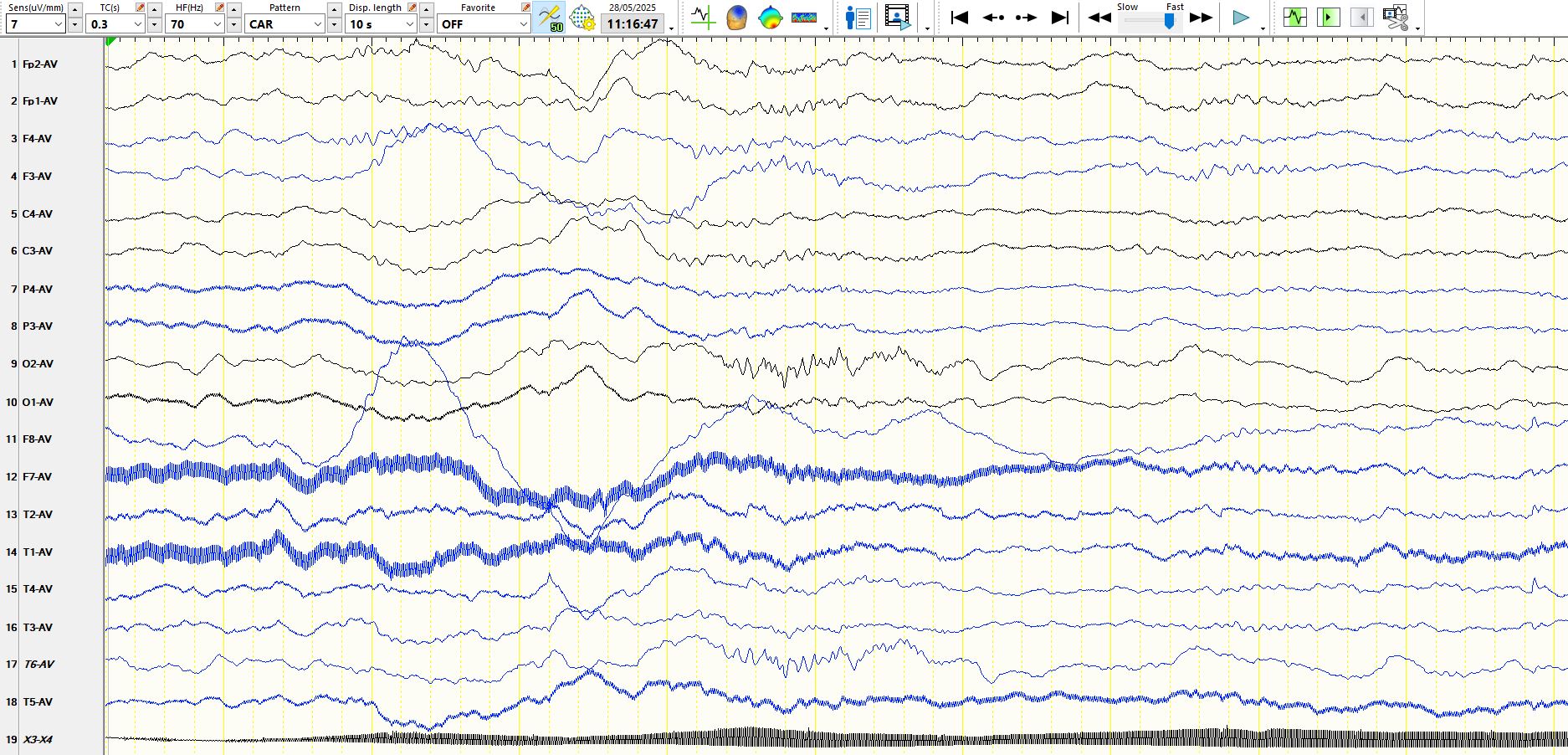
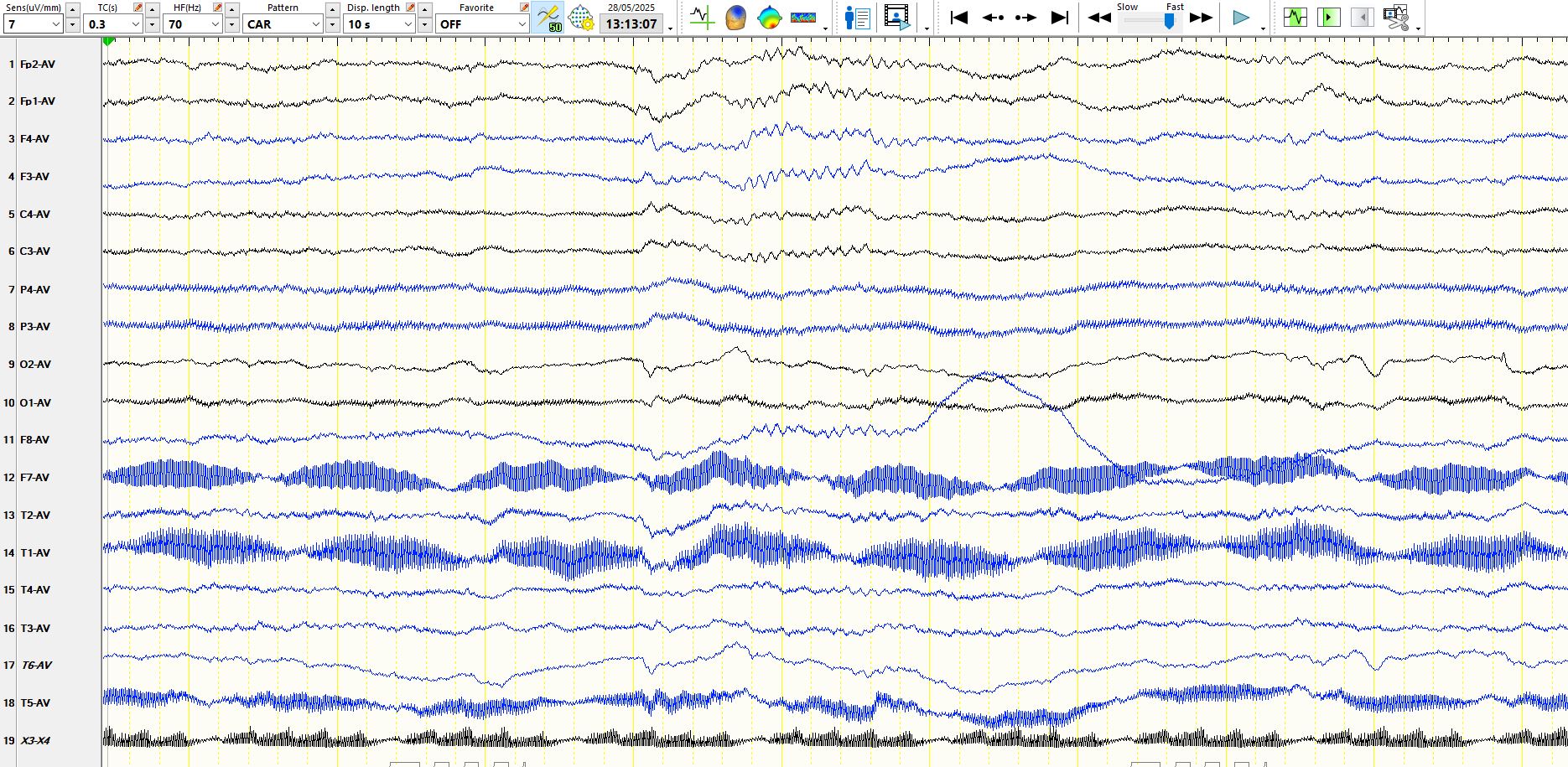
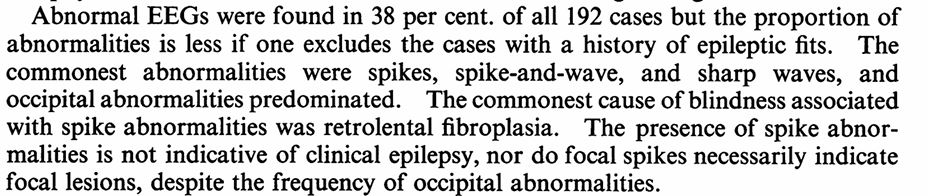
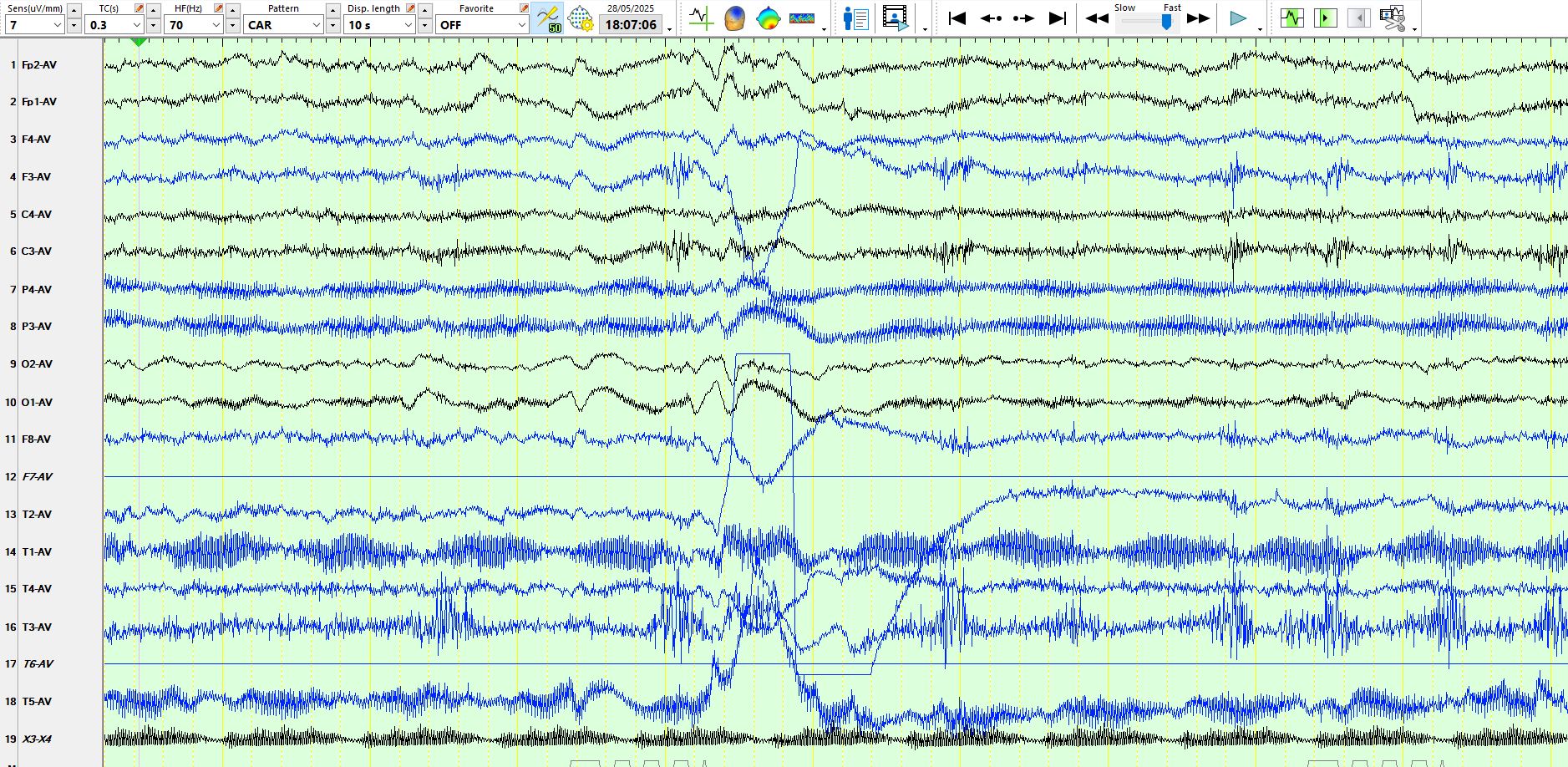
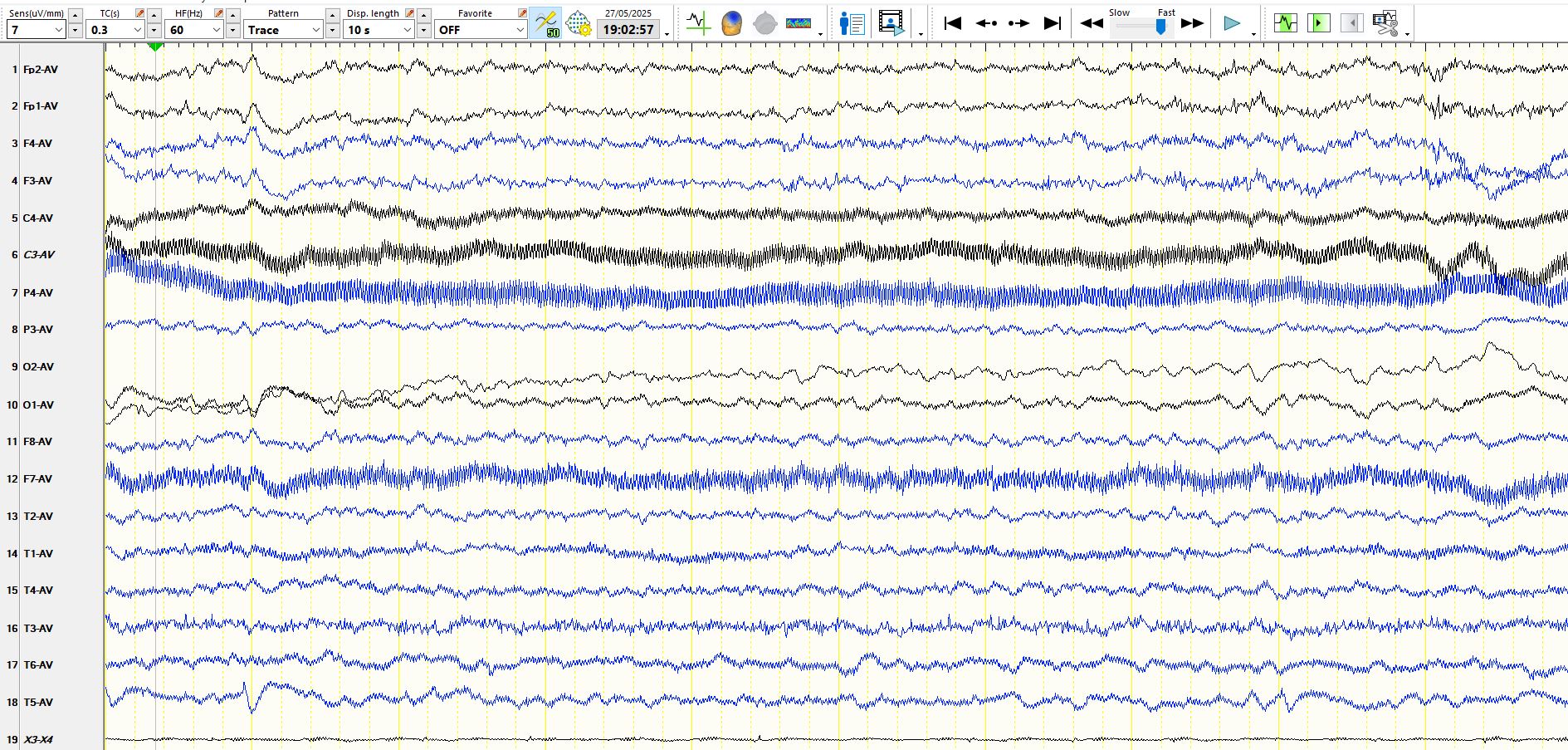
He has no alpha rhythms, there are intermittent delta waves over both occipital regions, sometimes with a triphasic morphology, which likely represent "fragments" of sharp and slow waves and bilateral, independent occipital sharp waves and spikes. These appear most abundantly, by some way, over the right occipital region. In sleep he often has long trains of periodic, rhythmic spike-and-wave at O2.
Here is another page of right occipital spikes:
Here are the trains of spikes in sleep
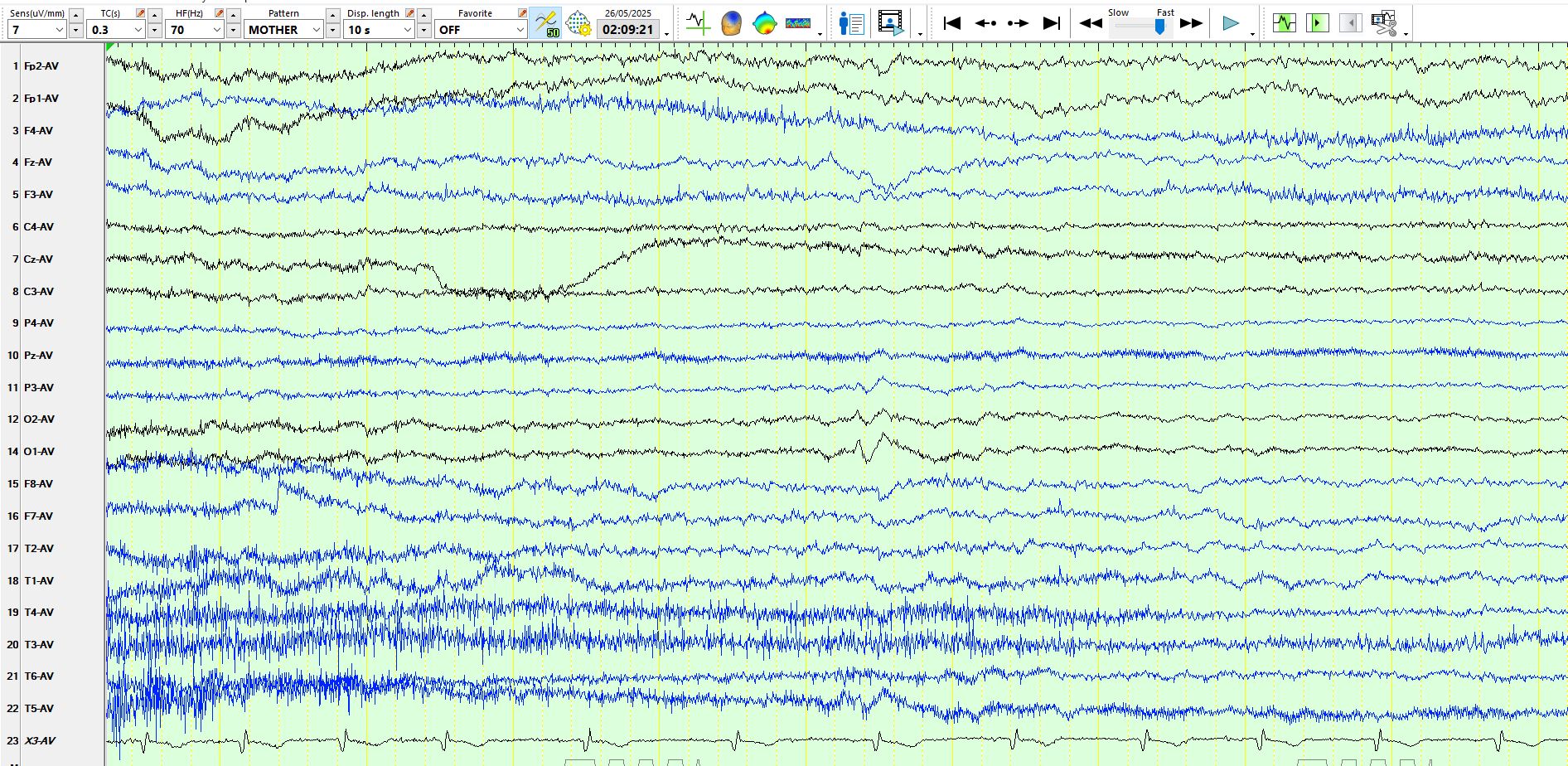
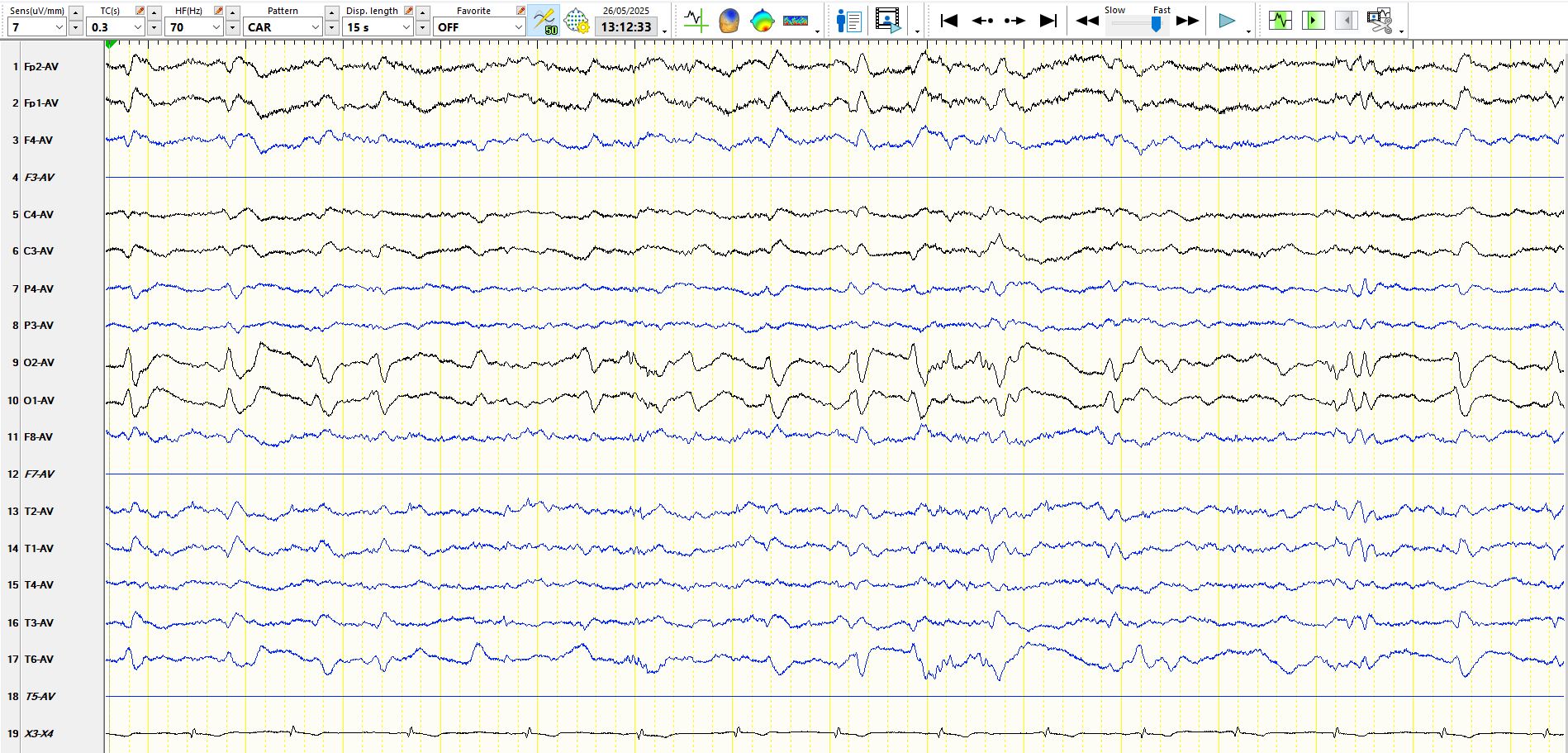
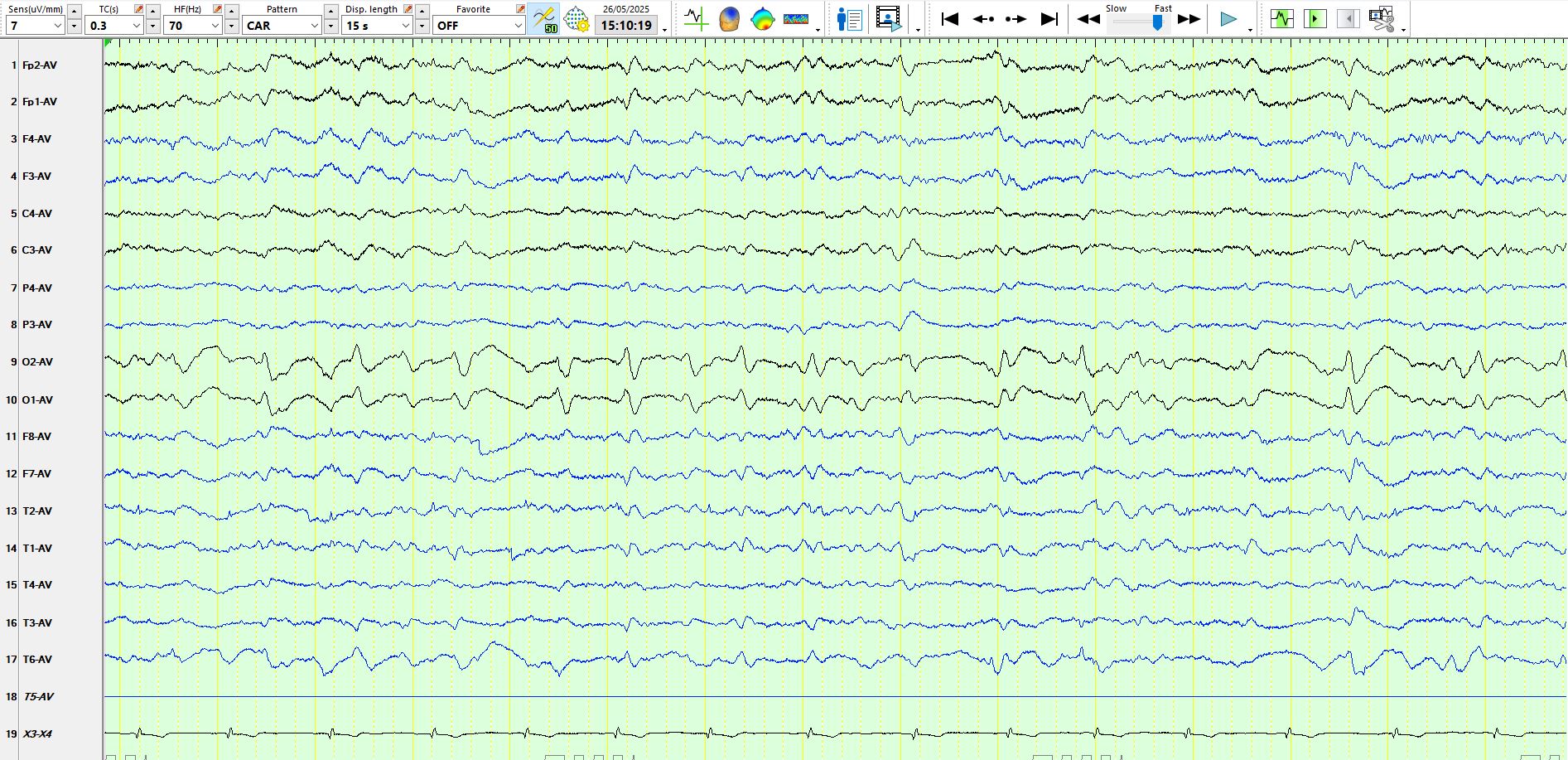
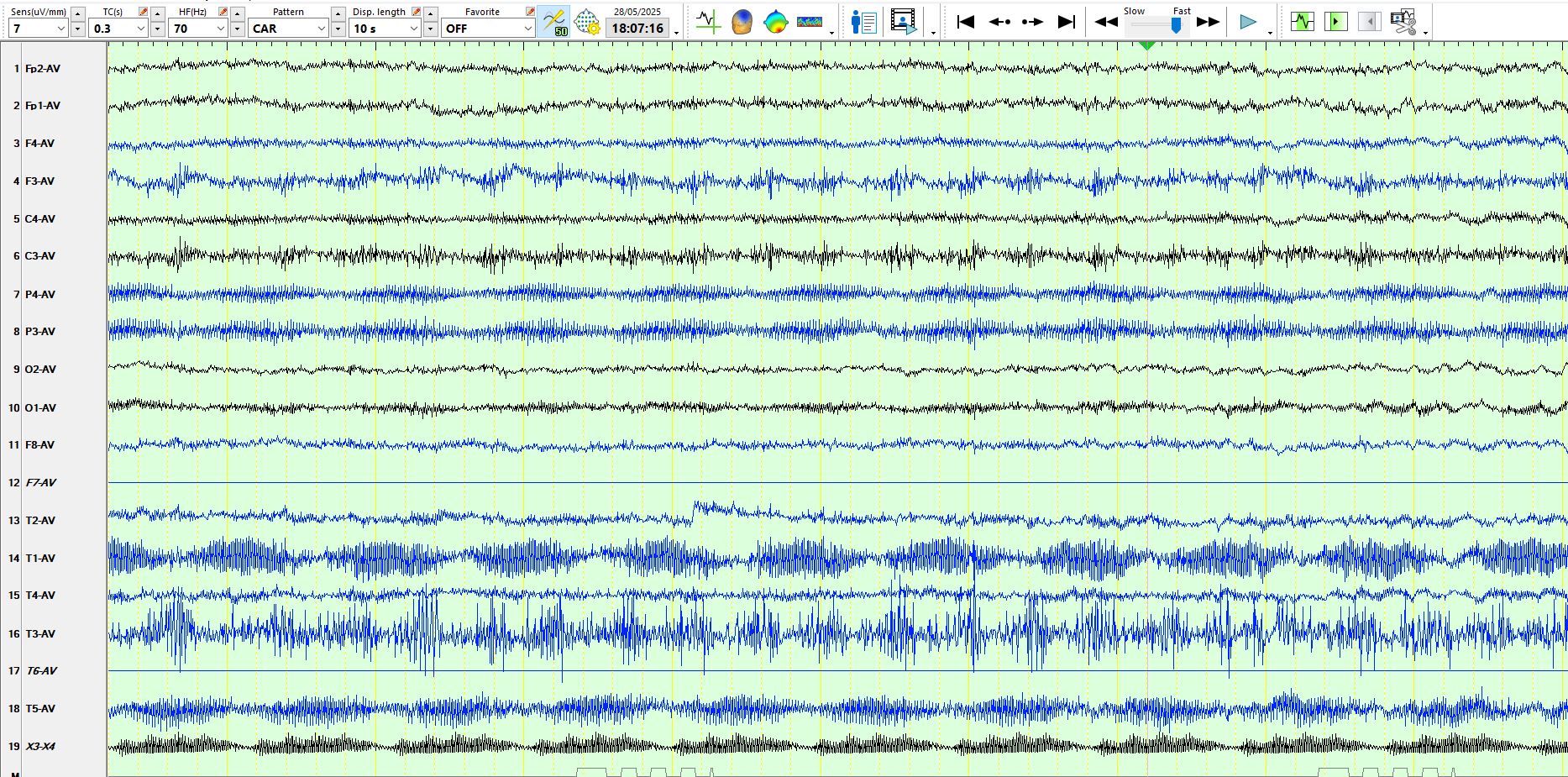
Here are alpha (and some beta) frequencies representing inter-ictal epileptiform discharges at O2:
The above are not spindles and here is an example of spindles from the same patient (See below):
Here are some references related to the above (if nothing else look at the abstracts)
Teaching NeuroImage: Needle-like Occipital Spikes in Children With Visual Impairment - PMC
Normal variants and artifacts: Importance in EEG interpretation - PubMed|
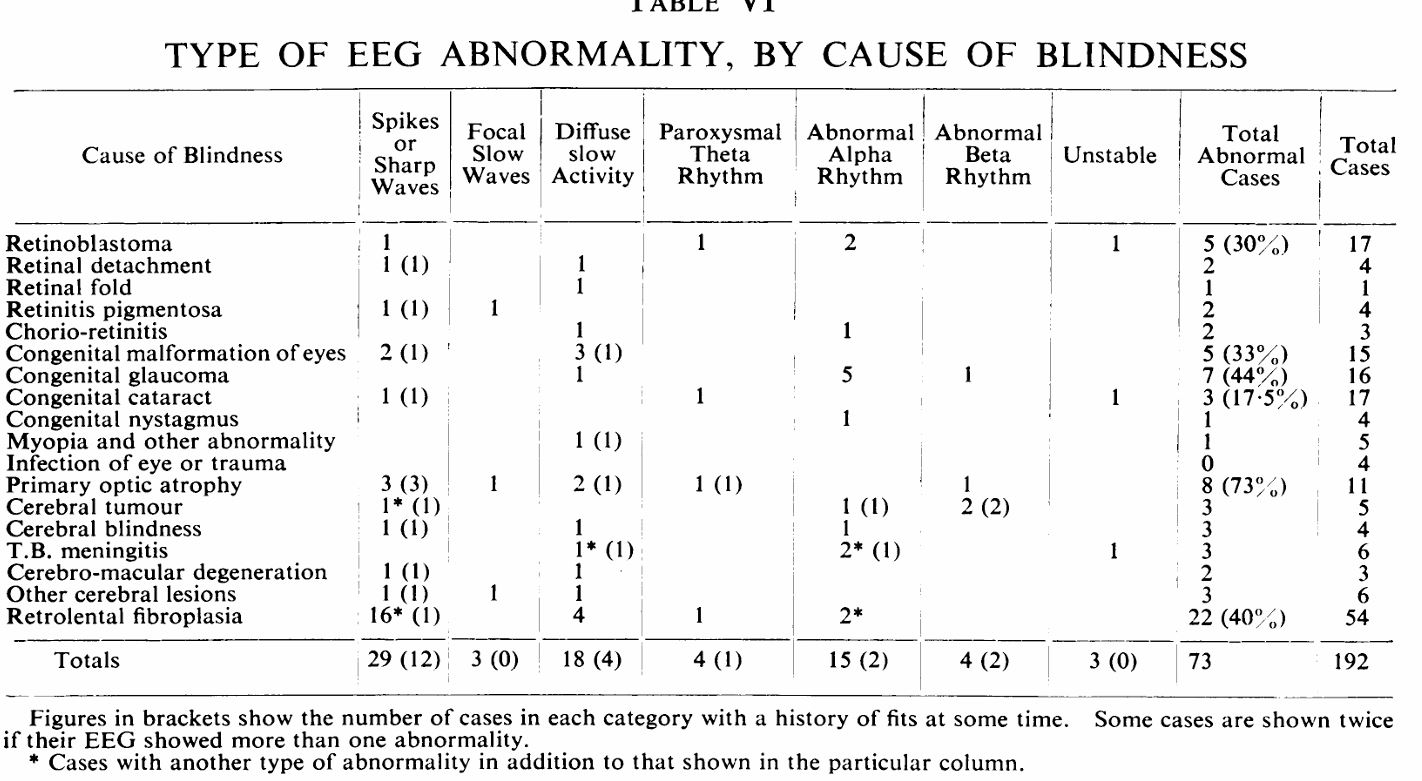
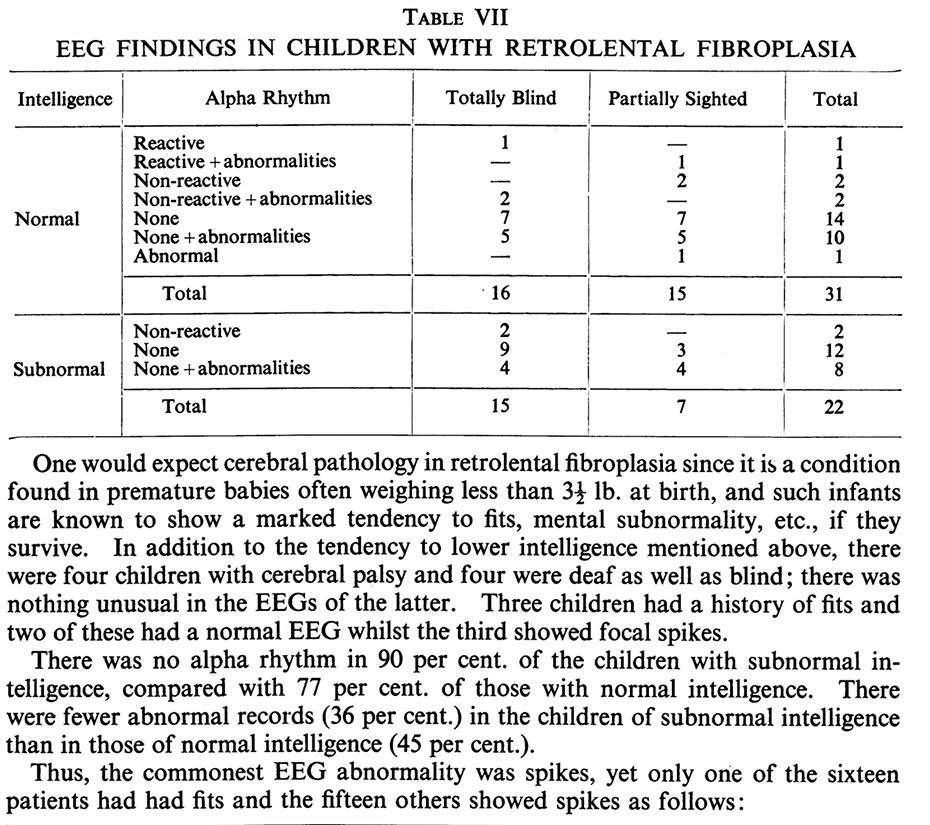
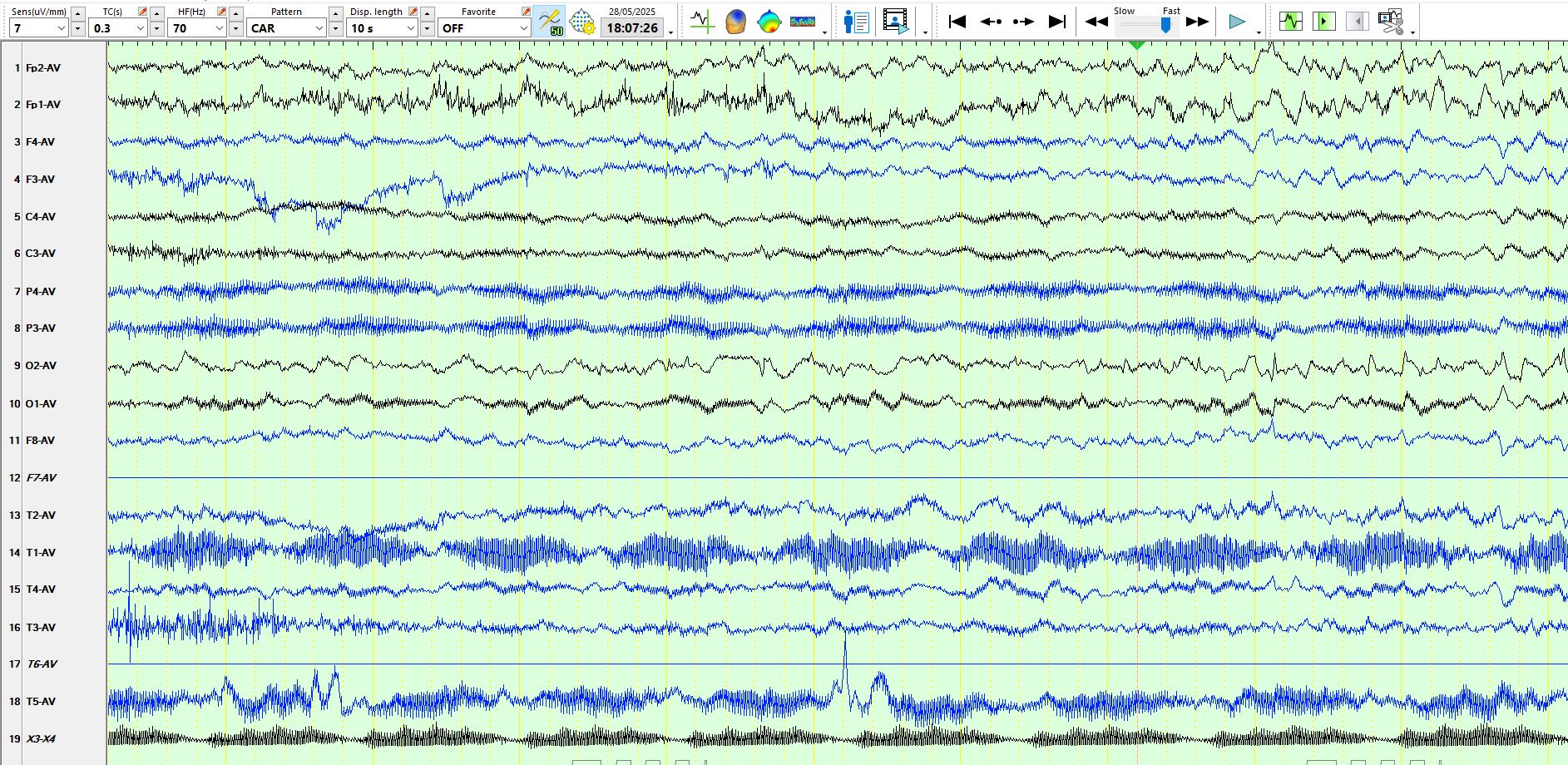
The following is the original description of the observation in blind children, published in 1964
brjopthal00386-0024.pdf
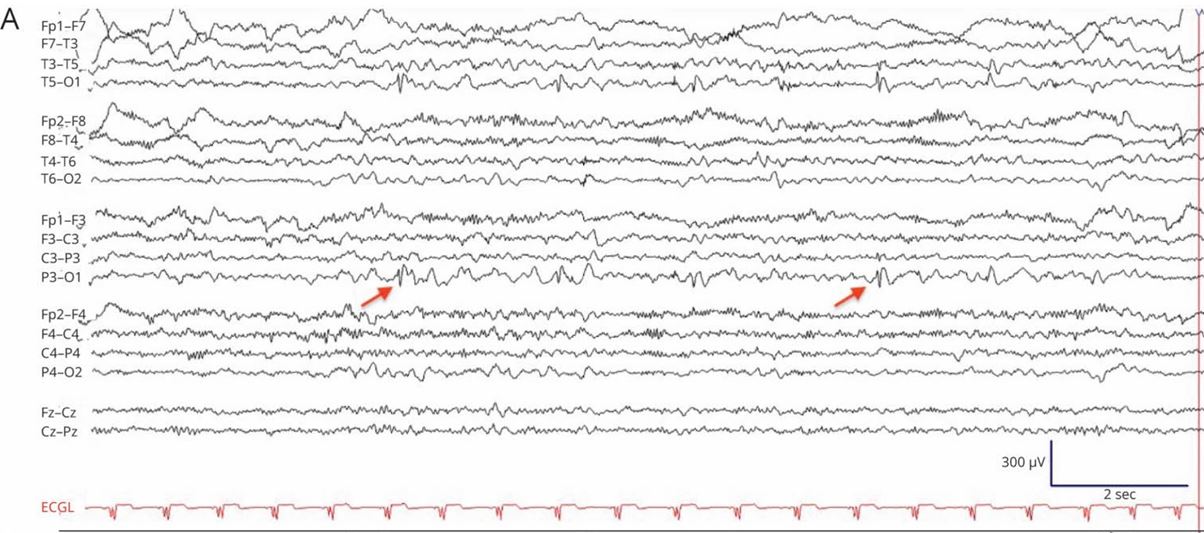
I must confess, I have never seen such spikes in blind people without seizures, and a Medline search reveals very little on the subject. The first article above is a case report of this, and a copy of such an EEG is taken from the first article above:
Here is a table from the original description by Jeavons in 1964.
The above is from the same article, 1964, Jeavons
While spikes were not associated with epileptic seizures most children, the mere fact that they did EEGs relatively early in life does not exclude the possibility that these discharges were part of epileptogenesis and that some/many/all would develop seizures later in life. The pertinent point is that spikes on an EEG, while commonly associated with the clinical diagnosis of epileptic seizures, in themselves do not prove that someone has epilepsy, let alone requiring treatment. Furthermore, clinical experience demonstrates that, in people diagnosed with epilepsy, the location of spikes does not prove the region of origin of seizures (people with extra temporal lobe epilepsy often have temporal spikes, multiple independent spikes foci may be associated with uni-focal originating seizures et cetera)
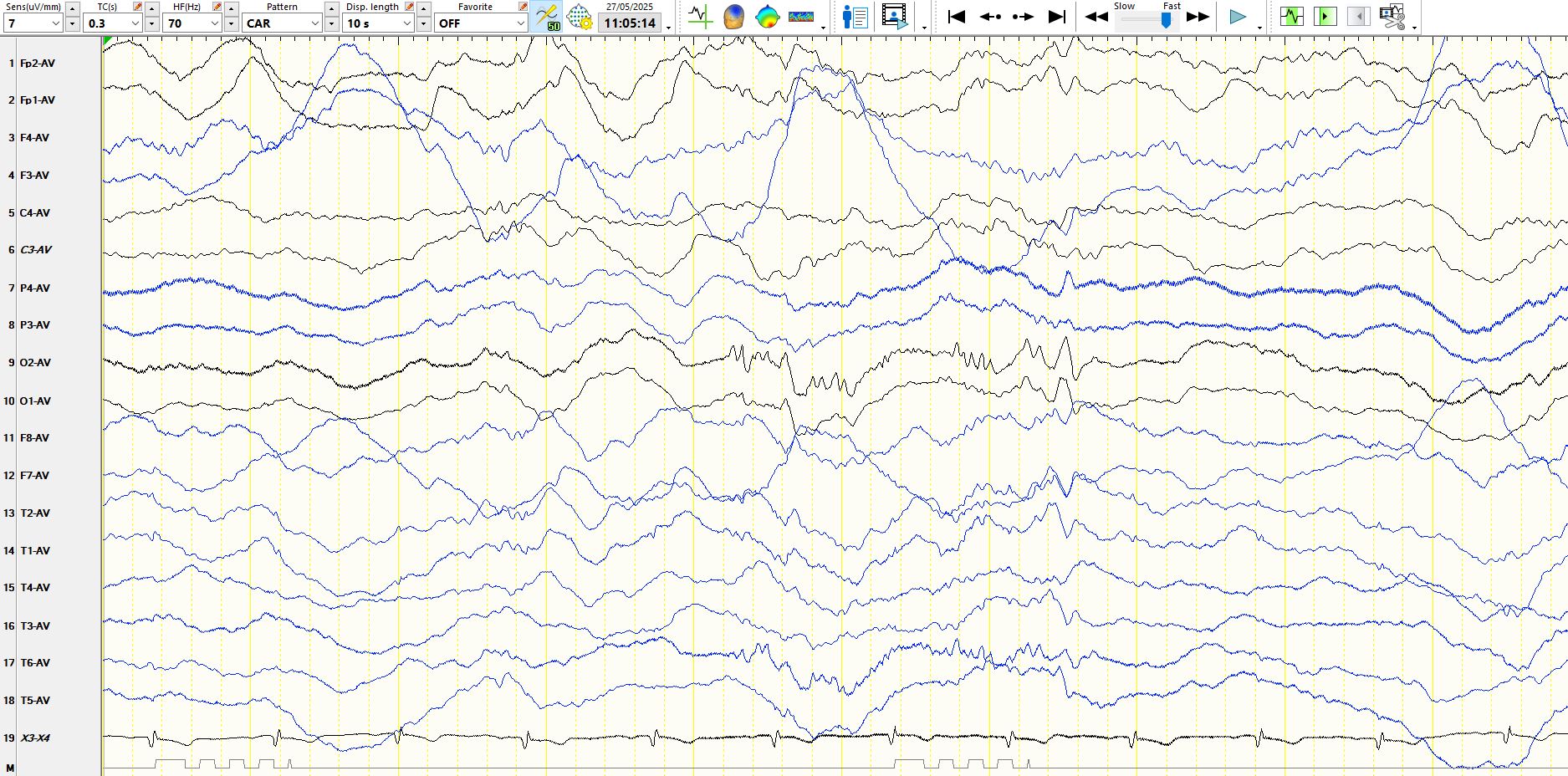
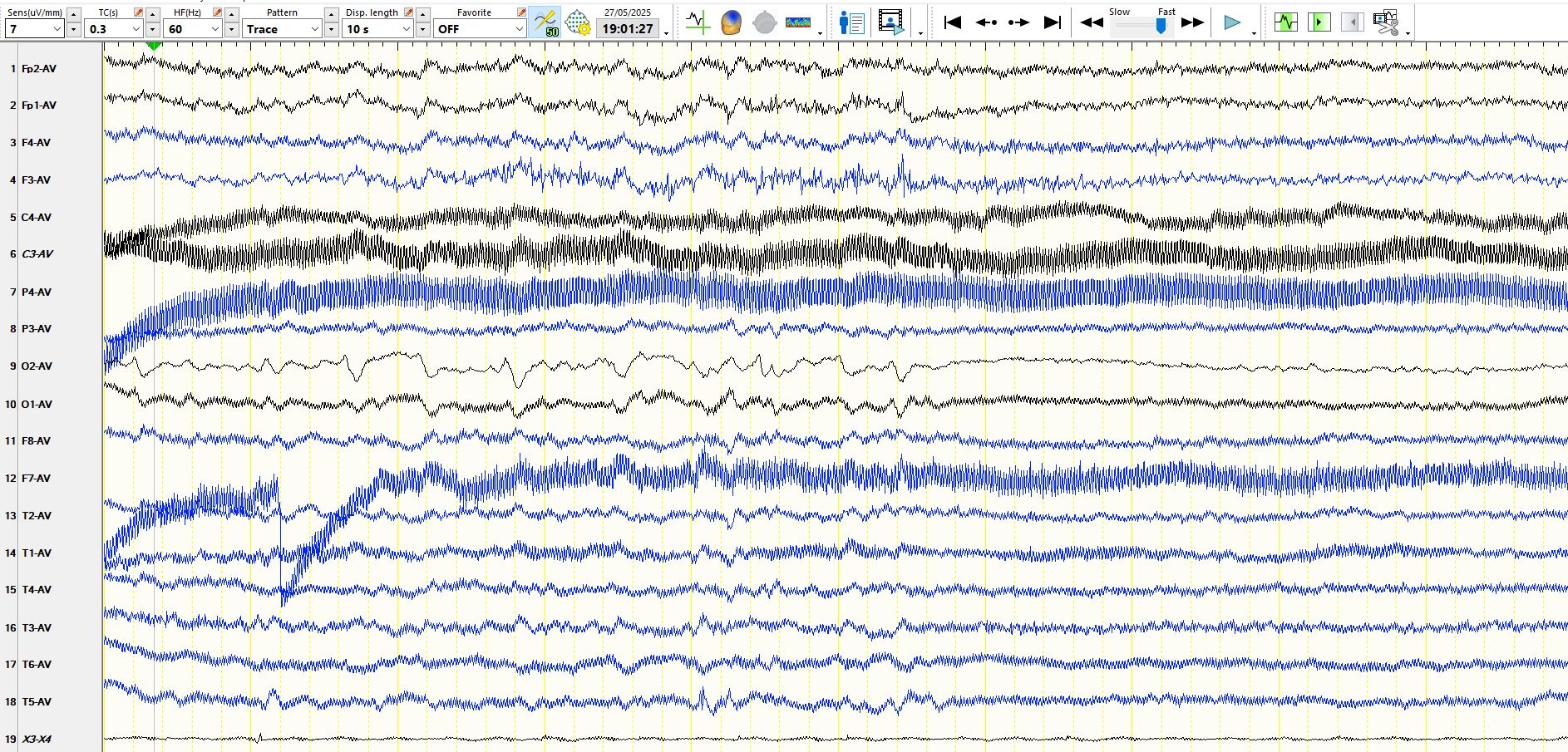
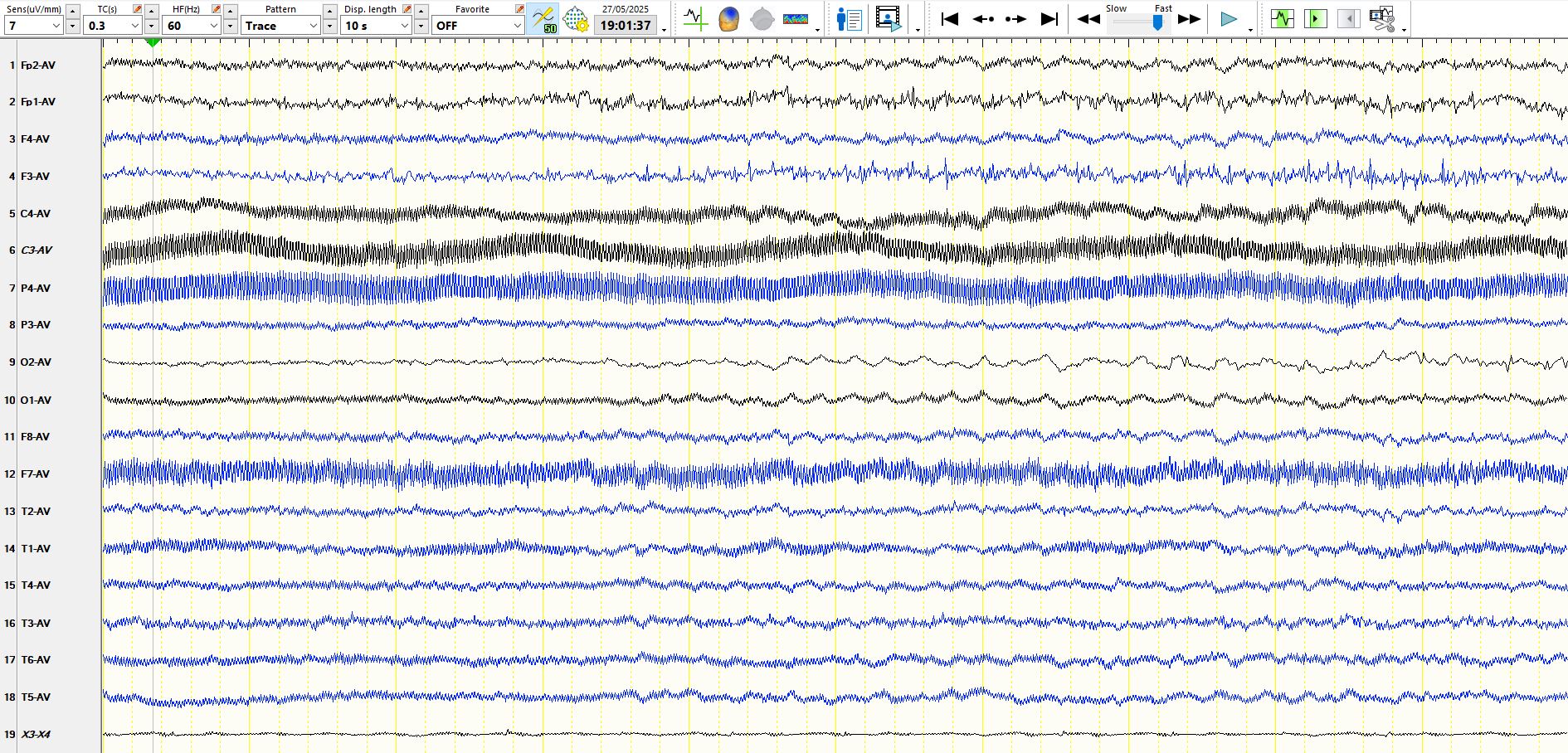
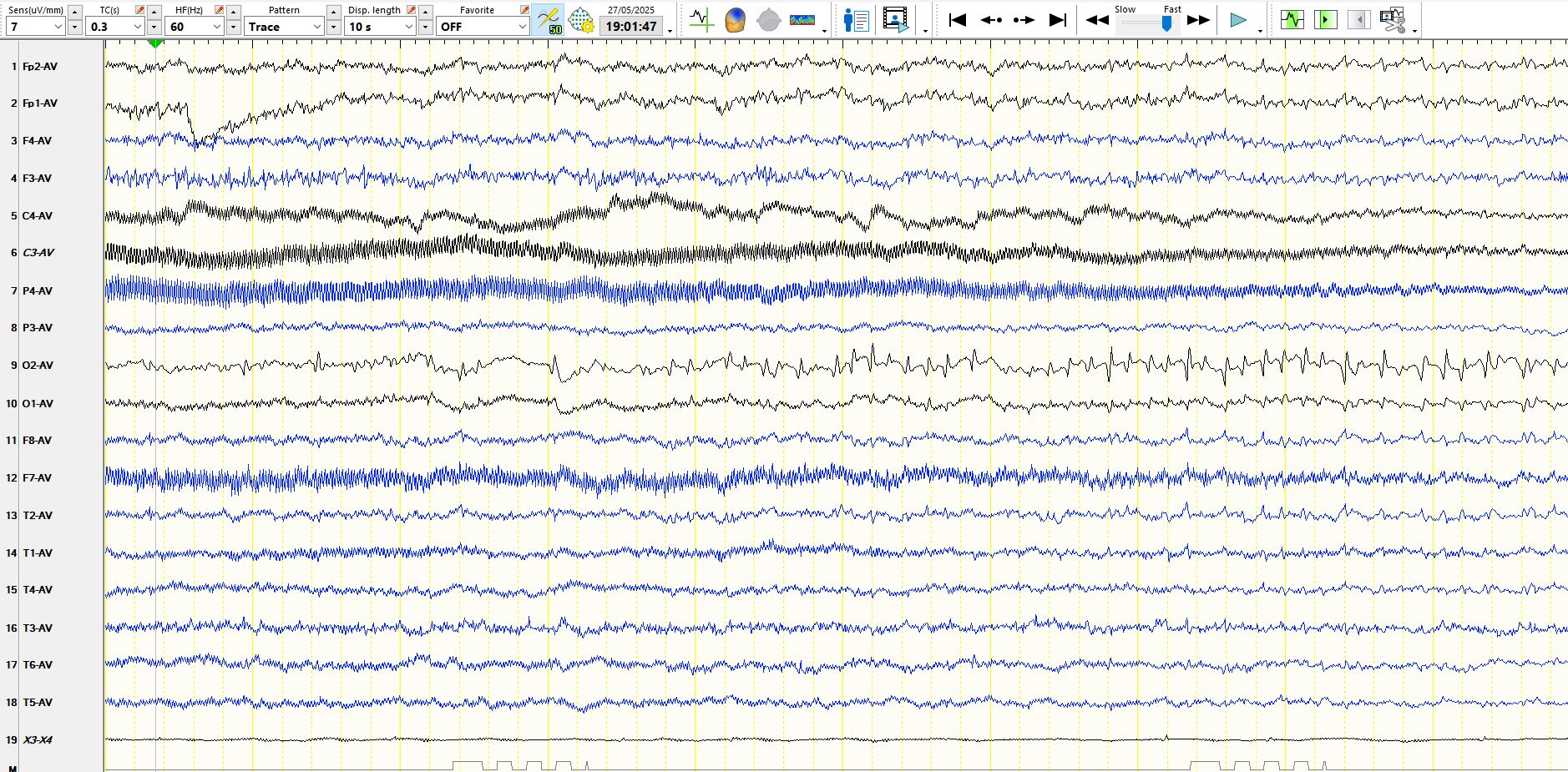
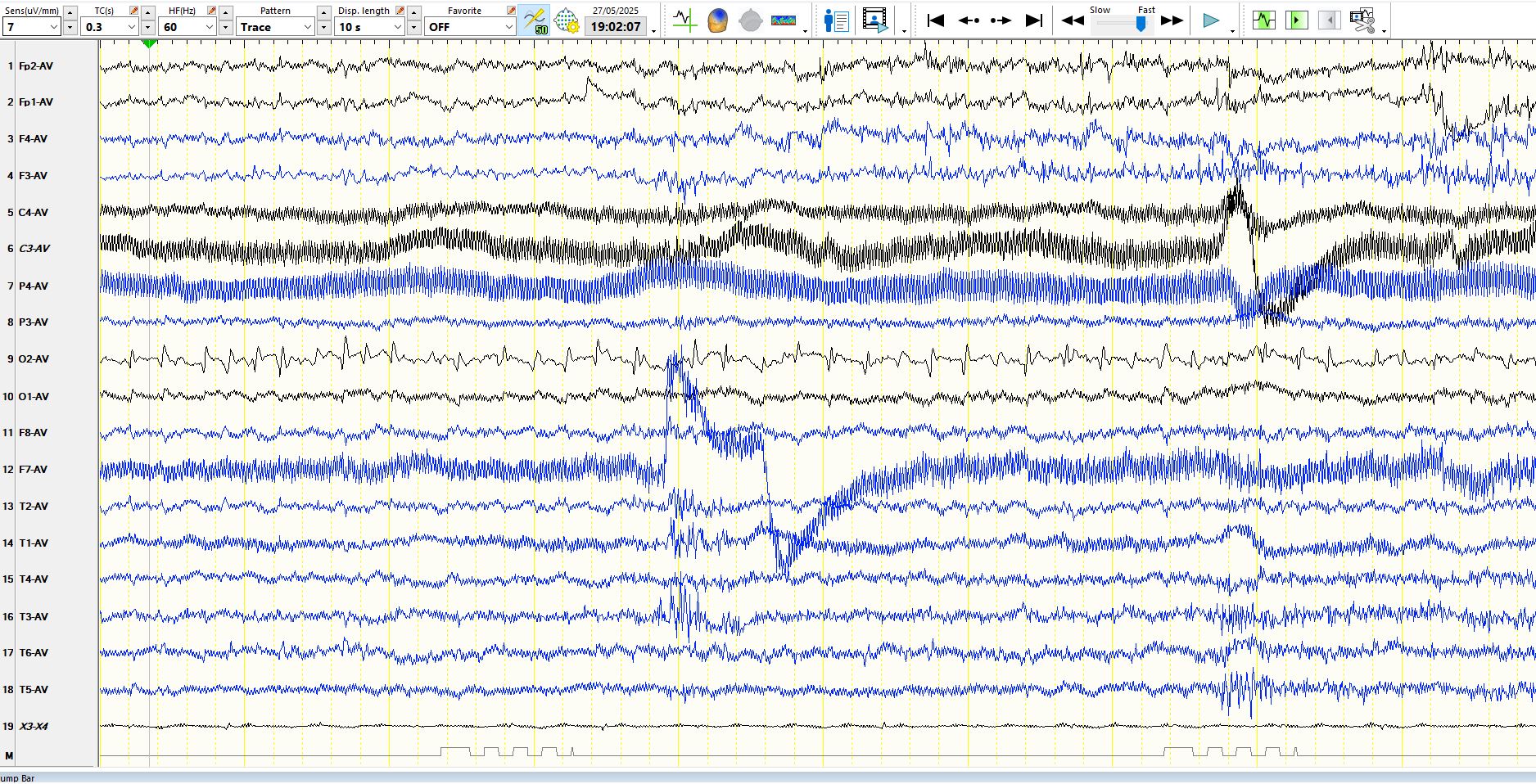
So, what about the patient presented at the introduction of this section? He has epilepsy and is able to distinguish between late and dark only (I did not test him on this), but I questioned him about unformed visual hallucinations at the start of his seizures or at other times and he reports none. His seizures are without warning and on EEG the onset looks as follows:
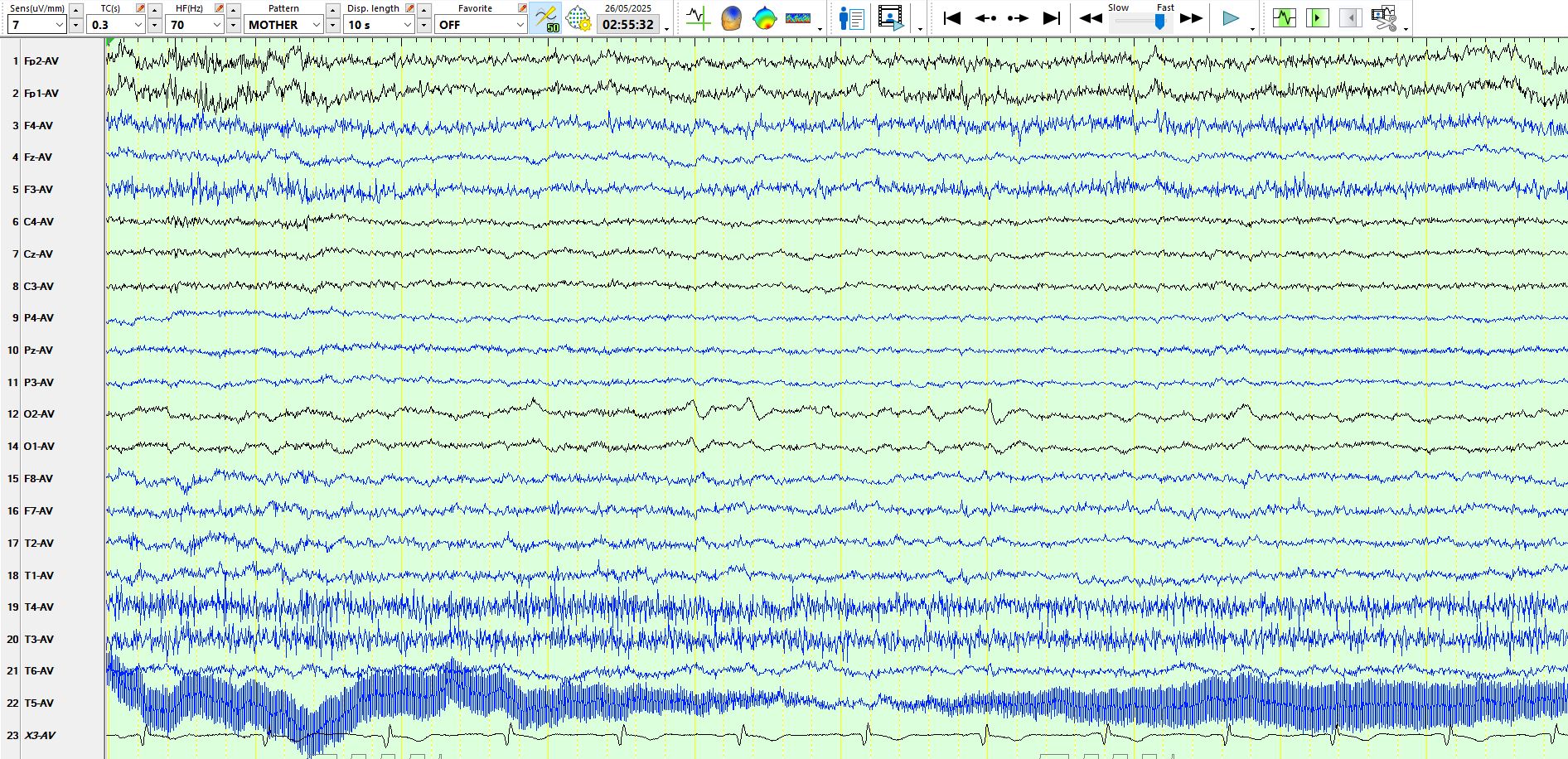
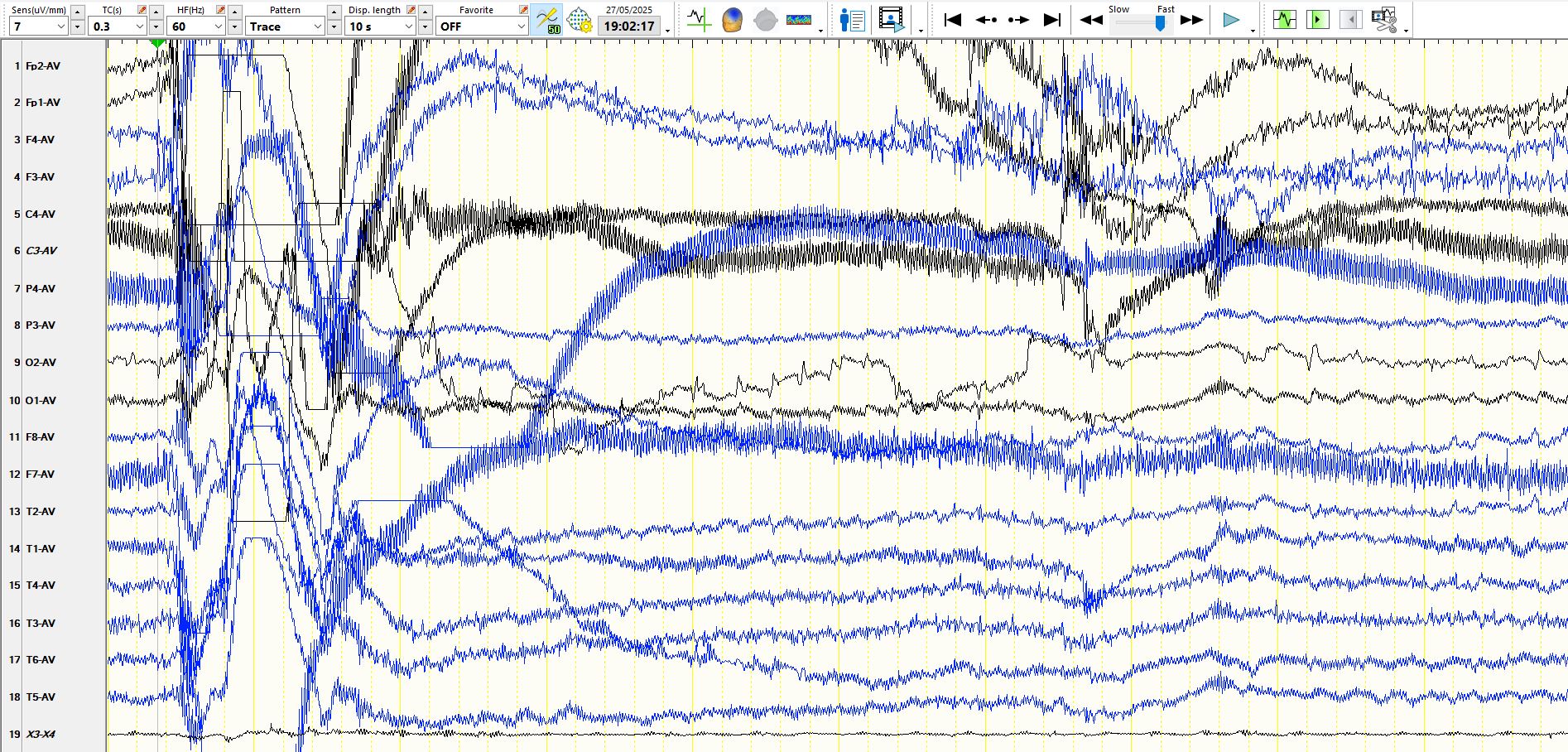
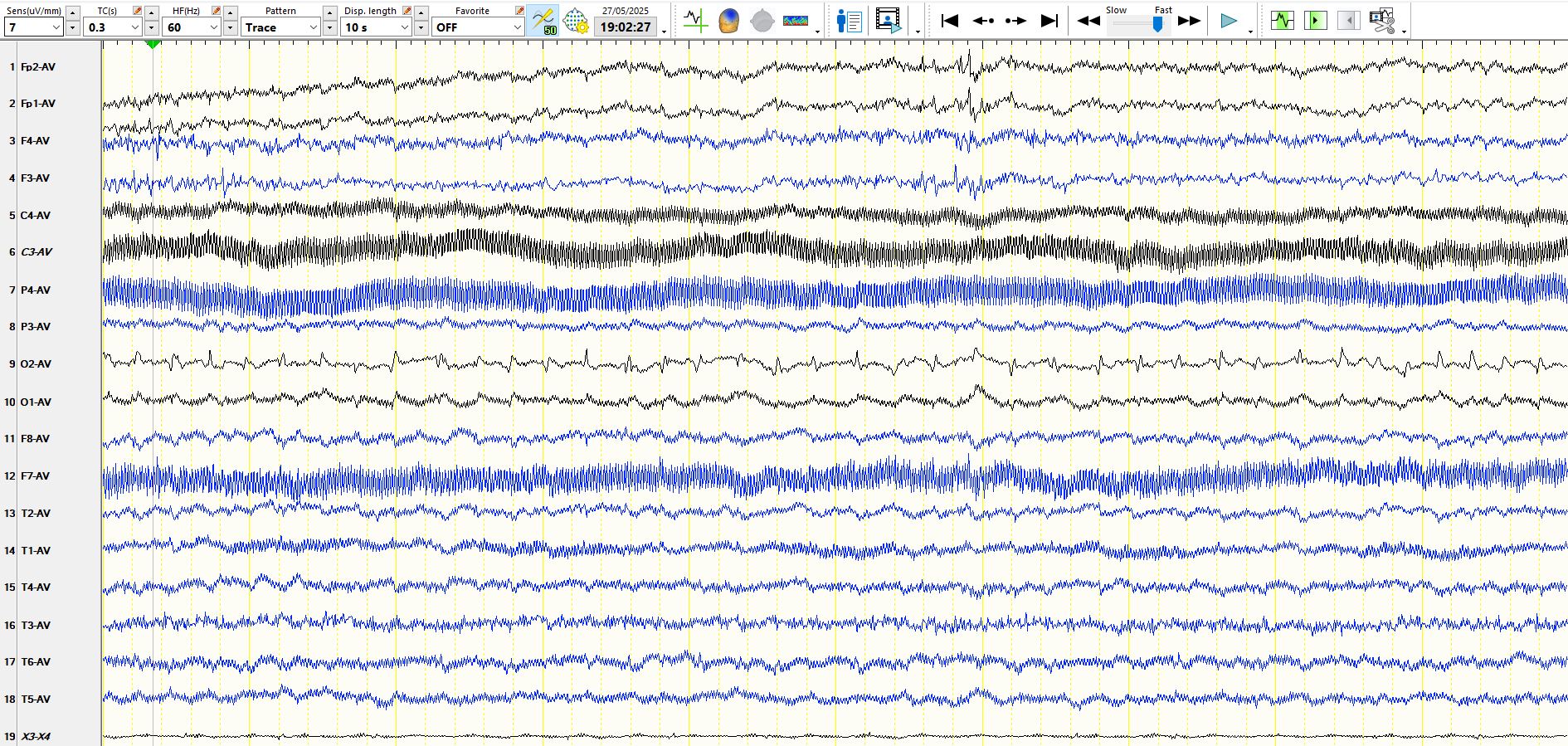
The first spiking appears approximately 15 seconds after the start of the seizure, which likely occurs when the EEG abruptly changes at about 4s on the first of the above three pages. Hence, given the inter-ictal findings and the earliest EEG changes, seizure likely originated somewhere in the right occipital region. About 10 seconds after the start of the spiking at O2, there is version of the head to the left, followed by asymmetric tonic posturing and late version of the head to the right. The issue of the reliability of version of the head as a subject in itself only: in short, it is an unreliable sign in general. There are specific circumstances in which it is very useful.
In addition to the single asymmetric tonic seizure, he had numerous subclinical seizures lasting up to 80 seconds, with no video correlate, during a few days of video-EEG recordings. You may then appreciate that the absence of a history of epileptic seizures does not preclude the possibility that someone has subclinical seizures, in this case prolonged. Hence, some and, who knows, maybe all of the children described by Jeavons had subclinical seizures that nobody ever knew about and as described above, perhaps some of these children were destined to have epilepsy later in life. Hence, notwithstanding the second reference above and other texts which regard these spikes in blind people as "normal variants", I would suggest that one should not regard these as "normal" and one should still classify them as inter-ictal epileptiform discharges in the same way that one would regard the finding of generalised spike-and-wave in an asymptomatic individual as someone carrying the genes for epilepsy, who may or may not have had subclinical seizures and who may or may not be destined to have epileptic seizures in the future.
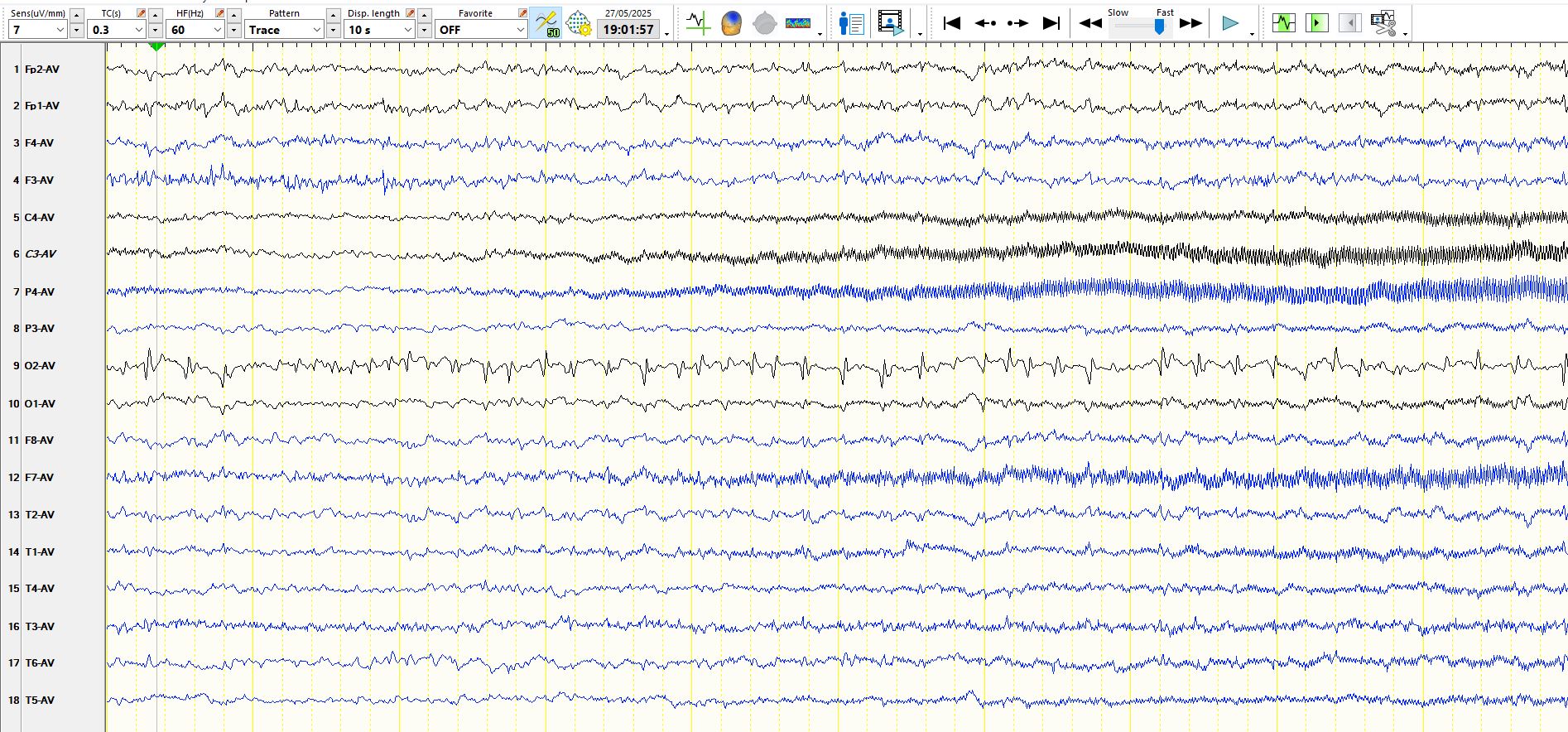
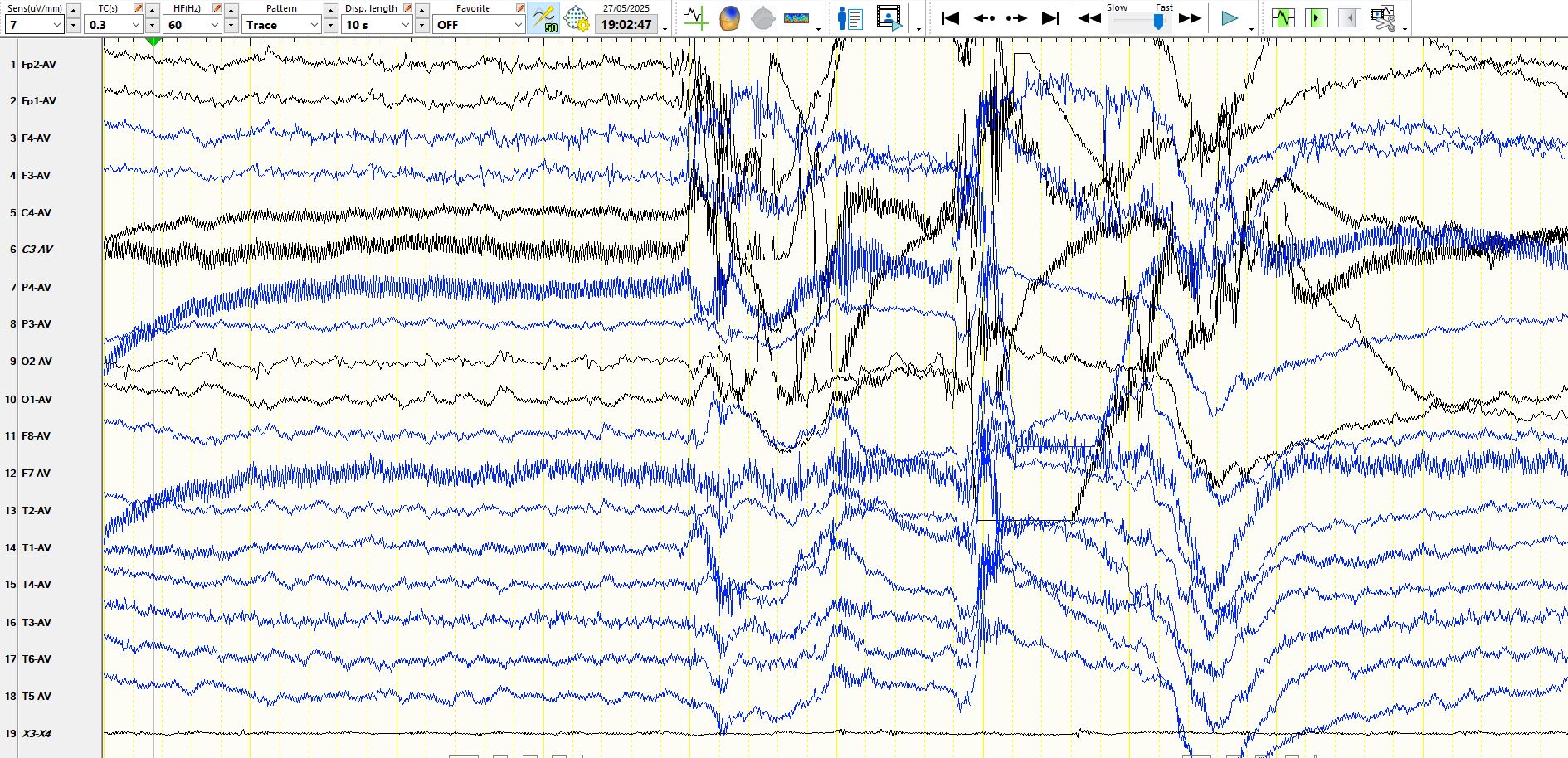
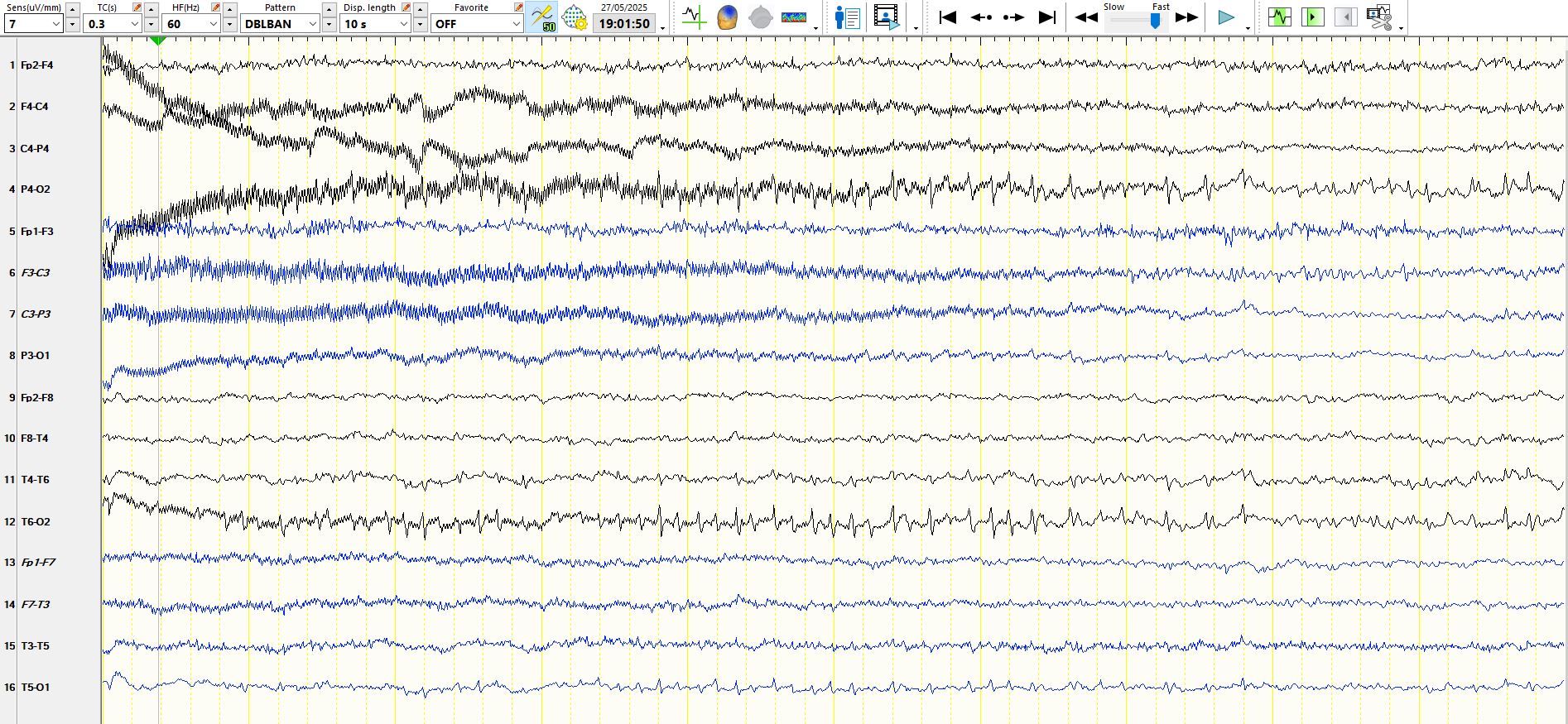
Here is an example of a long subclinical seizure that starts while he is awake and he lies quietly on his right-hand side throughout the event (of note, his family report no minor seizures, although on some days he is not quite his usual cheerful self):
The above discharge has a "biological field" and cannot be explained by any artefact. Just for good measure, here is a bipolar representation of one page of the seizure:
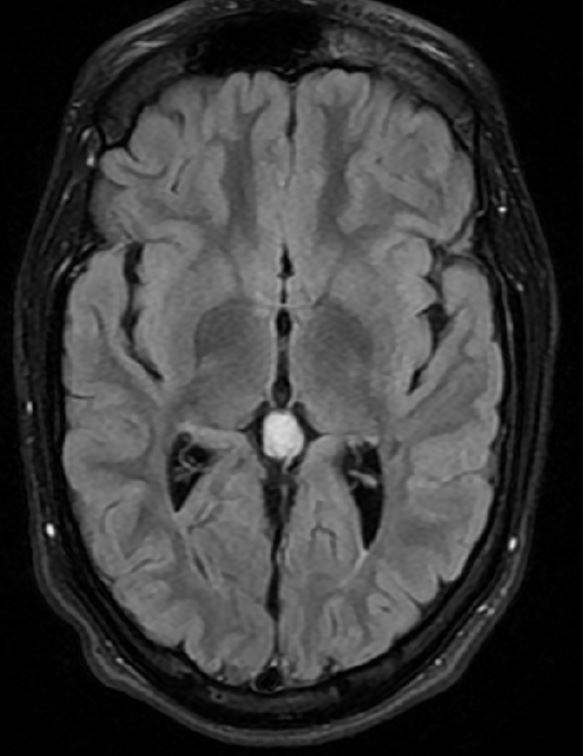
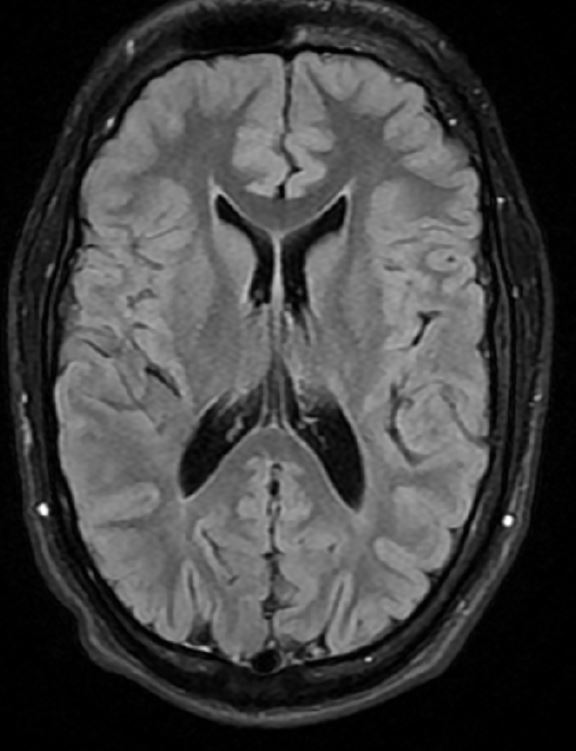
The MRI was reported as normal, but I think it shows thinning of white matter posteriorly, but no clear ulegyria:


After seven years of drug resistant seizures, he is currently being considered for epilepsy surgery.